J Korean Neuropsychiatr Assoc.
2013 Nov;52(6):409-416.
Factors Associated with the Compliance of Cognitive Behavioral Therapy for Obsessive Compulsive Disorder
- Affiliations
-
- 1Department of Neuropsychiatry, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Department of Neuropsychiatry, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea. kwonjs@snu.ac.kr
- 3Clinical Cognitive Neuroscience Center, Neuroscience Institute, SNU-MRC, Seoul, Korea.
- 4Department of Brain and Cognitive Sciences-WCU Program, College of Natural Sciences, Seoul National University, Seoul, Korea.
Abstract
OBJECTIVES
Non-completion rate of cognitive behavioral therapy (CBT) for Obsessive Compulsive Disorder (OCD) was reported to be higher than expected and it could interfere with the effectiveness of treatment. The aim of this study was to investigate predictors of treatment non-completion and to compare the effectiveness of CBT for OCD between completers and non-completers.
METHODS
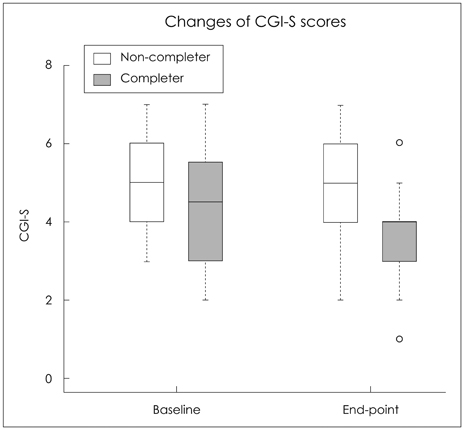
We studied 107 patients with a principal diagnosis of OCD who initiated a 13-week CBT for OCD from June 2004 to June 2011. Demographic and clinical characteristics, psychiatric co-morbidity, and medication of 20 participants who did not complete therapy were compared with those of treatment completers (n=87). Clinical Global Impression scores were also compared between the two groups in order to evaluate the effect of CBT for OCD at the 13th week.
RESULTS
The results showed a difference in marital status between treatment completers and non-completers : more non-completers were not married (p=0.04). Patients with aggressive obsessions at baseline showed a trend (p=0.06) toward lower treatment completion than those with only non-aggressive obsession. In addition, the non-completer group showed a trend of not being medicated (p=0.08). No other differences were observed between completers and non-completers. The 13th week Clinical Global Impression-Improvement scores were significantly different ; completers (2.5+/-0.8) and non-completers (3.2+/-0.8) (p<0.001).
CONCLUSION
In this study, we confirmed that CBT could affect symptom improvement of OCD and treatment non-completion interfered with effectiveness of CBT. However, in the current state of our knowledge, no factor is clinically applicable as a predictor of treatment non-completion. Therefore, these results suggest that clinicians should monitor compliance during CBT for OCD patients.
Keyword
MeSH Terms
Figure
Reference
-
1. American Psychiatry Association. Diagnostic and Statistical Manual of Mental Disorders. 4th edition. Washington, DC: American Psychiatry Association;1995.2. Horwath E, Weissman MM. The epidemiology and cross-national presentation of obsessive-compulsive disorder. Psychiatr Clin North Am. 2000; 23:493–507.
Article3. Goodman WK, Price LH, Rasmussen SA, Delgado PL, Heninger GR, Charney DS. Efficacy of fluvoxamine in obsessive-compulsive disorder. A double-blind comparison with placebo. Arch Gen Psychiatry. 1989; 46:36–44.
Article4. Anand N, Sudhir PM, Math SB, Thennarasu K, Janardhan Reddy YC. Cognitive behavior therapy in medication non-responders with obsessive-compulsive disorder: a prospective 1-year follow-up study. J Anxiety Disord. 2011; 25:939–945.
Article5. Abramowitz JS. The psychological treatment of obsessive-compulsive disorder. Can J Psychiatry. 2006; 51:407–416.
Article6. Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, et al. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 2005; 162:151–161.
Article7. Mancebo MC, Pinto A, Rasmussen SA, Eisen JL. Development of the Treatment Adherence Survey-patient version (TAS-P) for OCD. J Anxiety Disord. 2008; 22:32–43.
Article8. Mancebo MC, Eisen JL, Pinto A, Greenberg BD, Dyck IR, Rasmussen SA. The brown longitudinal obsessive compulsive study: treatments received and patient impressions of improvement. J Clin Psychiatry. 2006; 67:1713–1720.9. Belotto-Silva C, Diniz JB, Malavazzi DM, Valério C, Fossaluza V, Borcato S, et al. Group cognitive-behavioral therapy versus selective serotonin reuptake inhibitors for obsessive-compulsive disorder: a practical clinical trial. J Anxiety Disord. 2012; 26:25–31.
Article10. Simpson HB, Maher MJ, Wang Y, Bao Y, Foa EB, Franklin M. Patient adherence predicts outcome from cognitive behavioral therapy in obsessive-compulsive disorder. J Consult Clin Psychol. 2011; 79:247–252.
Article11. Diniz JB, Malavazzi DM, Fossaluza V, Belotto-Silva C, Borcato S, Pimentel I, et al. Risk factors for early treatment discontinuation in patients with obsessive-compulsive disorder. Clinics (Sao Paulo). 2011; 66:387–393.
Article12. Mancebo MC, Eisen JL, Sibrava NJ, Dyck IR, Rasmussen SA. Patient utilization of cognitive-behavioral therapy for OCD. Behav Ther. 2011; 42:399–412.
Article13. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I disorder. New York: New York Psychiatric Institute;1996.14. First MB, Donovan S, Frances A. Nosology of chronic mood disorders. Psychiatr Clin North Am. 1996; 19:29–39.
Article15. Jónsson H, Hougaard E. Group cognitive behavioural therapy for obsessive-compulsive disorder: a systematic review and meta-analysis. Acta Psychiatr Scand. 2009; 119:98–106.
Article16. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989; 46:1006–1011.17. Steer RA, Rissmiller DJ, Ranieri WF, Beck AT. Structure of the computer-assisted Beck Anxiety Inventory with psychiatric inpatients. J Pers Assess. 1993; 60:532–542.
Article18. Gorenstein C, Andrade L. Validation of a Portuguese version of the Beck Depression Inventory and the State-Trait Anxiety Inventory in Brazilian subjects. Braz J Med Biol Res. 1996; 29:453–457.19. Kozak MJ, Foa EB. Mastery of obsessive compulsive disorder : A Cognitive-Behavioral Approach. Therapy Works, Inc;1997.20. Rachman S, Thordarson DS, Shafran R, Woody SR. Perceived responsibility: structure and significance. Behav Res Ther. 1995; 33:779–784.
Article21. Salkovskis PM, Warwick H. Cognitive therapy of obsessive-compulsive disorder: treating treatment failures. Behav Psychother. 1985; 13:243–255.
Article22. Salkovskis PM. Understanding and treating obsessive-compulsive disorder. Behav Res Ther. 1999; 37:Suppl 1. S29–S52.
Article23. Guy W. Clinical Global Impressions (CGI) scale. In : Rush J, First MB, Blacker D, editors. Handbook of psychiatric measures. 2nd ed. New Delhi: American Psychiatric Publishing;2010. p. 90–92.24. Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D, et al. The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry. 2006; 11:495–504.
Article25. Jaurrieta N, Jiménez-Murcia S, Alonso P, Granero R, Segalàs C, Labad J, et al. Individual versus group cognitive behavioral treatment for obsessive-compulsive disorder: follow up. Psychiatry Clin Neurosci. 2008; 62:697–704.
Article26. Lippens T, Mackenzie CS. Treatment satisfaction, perceived treatment effectiveness, and dropout among older users of mental health services. J Clin Psychol. 2011; 67:1197–1209.
Article27. Santana L, Fontenelle JM, Yücel M, Fontenelle LF. Rates and correlates of nonadherence to treatment in obsessive-compulsive disorder. J Psychiatr Pract. 2013; 19:42–53.
Article28. Anand N, Sudhir PM, Math SB, Thennarasu K, Janardhan Reddy YC. Cognitive behavior therapy in medication non-responders with obsessive-compulsive disorder: a prospective 1-year follow-up study. J Anxiety Disord. 2011; 25:939–945.
Article29. Maher MJ, Huppert JD, Chen H, Duan N, Foa EB, Liebowitz MR, et al. Moderators and predictors of response to cognitive-behavioral therapy augmentation of pharmacotherapy in obsessive-compulsive disorder. Psychol Med. 2010; 40:2013–2023.
Article30. Prasko J, Raszka M, Adamcova K, Grambal A, Koprivova J, Kudrnovská H, et al. Predicting the therapeutic response to cognitive behavioural therapy in patients with pharmacoresistant obsessive-compulsive disorder. Neuro Endocrinol Lett. 2009; 30:615–623.31. Simpson HB, Liebowitz MR. Combining pharmacotherapy and cognitive-behavioral therapy in the treatment of OCD. In : Abramowitz JS, Houts AC, editors. Concepts and Controversies in Obsessive-Compulsive Disorder. New York: Springer;2005. p. 359–376.32. Franklin ME, Abramowitz JS, Kozak MJ, Levitt JT, Foa EB. Effectiveness of exposure and ritual prevention for obsessive-compulsive disorder: randomized compared with nonrandomized samples. J Consult Clin Psychol. 2000; 68:594–602.
Article33. Gava I, Barbui C, Aguglia E, Carlino D, Churchill R, De Vanna M, et al. Psychological treatments versus treatment as usual for obsessive compulsive disorder (OCD). Cochrane Database Syst Rev. 2007; (2):CD005333.
Article34. Anholt GE, Aderka IM, van Balkom AJ, Smit JH, Hermesh H, de Haan E, et al. The impact of depression on the treatment of obsessivecompulsive disorder: results from a 5-year follow-up. J Affect Disord. 2011; 135:201–207.
Article35. Andouz Z, Dolatshahi B, Moshtagh N, Dadkhah A. The efficacy of metacognitive therapy on patients suffering from pure obsession. Iran J Psychiatry. 2012; 7:11–21.36. Maher MJ, Wang Y, Zuckoff A, Wall MM, Franklin M, Foa EB, et al. Predictors of patient adherence to cognitive-behavioral therapy for obsessive-compulsive disorder. Psychother Psychosom. 2012; 81:124–126.
Article37. Eskildsen A, Hougaard E, Rosenberg NK. Pre-treatment patient variables as predictors of drop-out and treatment outcome in cognitive behavioural therapy for social phobia: A systematic review. Nord J Psychiatry. 2010; 64:94–105.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Korean Treatment Algorithm for Obsessive-Compulsive Disorder 2007(III): A Preliminary Study for Application of Cognitive-Behavioral Therapy
- Obsessive-Compulsive Disorder
- Aripiprazole Improved Obsessive Compulsive Symptoms in Asperger's Disorder
- Virtual Reality for Obsessive-Compulsive Disorder: Past and the Future
- The form and content of obsessions and compulsions in the obsessive-compulsive disorder