J Korean Neuropsychiatr Assoc.
2012 Sep;51(5):312-317.
Patterns of Drug Use and Factors Associated with Polypharmacy in Elderly Patients Visiting Psychiatric Outpatient Clinic
- Affiliations
-
- 1Department of Psychiatry, Inje University College of Medicine, Ilsan Paik Hospital, Goyang, Korea. intuit@paik.ac.kr
Abstract
OBJECTIVES
The objective of this study was to investigate the patterns and recent trends in polypharmacy among elderly patients visiting psychiatric outpatient clinic.
METHODS
289 elderly patients visiting psychiatric outpatient clinic were interviewed and their medical records were thoroughly reviewed. Inclusion criteria were as follows : 1) 65 years and older age patients, 2) diagnosed with one or more psychiatric disorder according to ICD-10 criteria, 3) who were willing to participate in this research. Demographic data and clinical data, including prevalence of polypharmacy, doses and types of drugs both prescribed and self-administered, were analyzed. Polypharmacy was defined as the long-term simultaneous use of six or more drugs. Data were statistically analyzed by t-test, analysis of variance, and simple regression analysis.
RESULTS
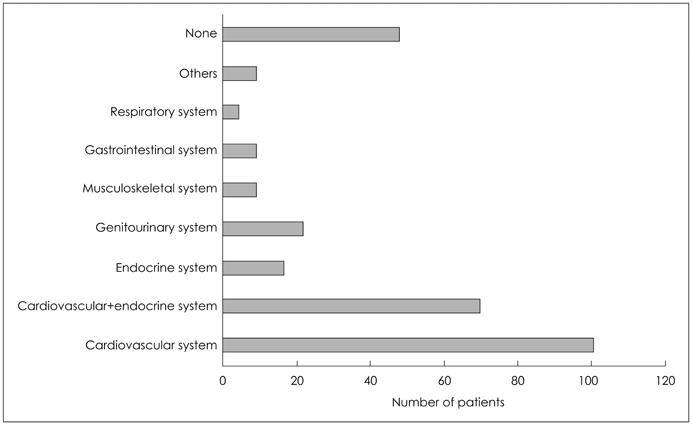
57.1% of the patients were prescribed with more than six drugs simultaneously. Mean number [+/-standard deviation (SD)] of psychiatric drug was 3.42+/-1.41. Prevalence of polyphamacy was different among psychiatric disorder groups, bipolar disorder group being the highest (mean+/-SD drug used=5.17+/-0.98). Regarding sedative-hypnotics, 59.5% of patients were prescribed (mean+/-SD drug used=2.02+/-1.07). Visual Analogue Scale (VAS) and total number of drugs prescribed were positively correlated (p<0.05). Herb medicine/dietary supplement had no influence on total number of used drugs.
CONCLUSION
Elderly patients are suffering from many comorbidities and vulnerable to multiple drug use that can be potentially harmful, so it is important and essential to be aware of the possibility of polypharmacy and prescribe appropriate drugs to improve their quality of life.
Keyword
MeSH Terms
Figure
Reference
-
1. Stahl SM, Grady MM. A critical review of atypical antipsychotic utilization: comparing monotherapy with polypharmacy and augmentation. Curr Med Chem. 2004. 11:313–327.
Article2. Fulton MM, Allen ER. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract. 2005. 17:123–132.
Article3. Jyrkkä J, Enlund H, Korhonen MJ, Sulkava R, Hartikainen S. Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons: results of the Kuopio 75+ study: a cross-sectional analysis. Drugs Aging. 2009. 26:493–503.
Article4. Kuijpers MA, van Marum RJ, Egberts AC, Jansen PA. OLDY (OLd people Drugs & dYsregulations) Study Group. Relationship between polypharmacy and underprescribing. Br J Clin Pharmacol. 2008. 65:130–133.
Article5. Zubenko GS, Sunderland T. Geriatric psychopharmacology: why does age matter? Harv Rev Psychiatry. 2000. 7:311–333.
Article6. Gören JL, Parks JJ, Ghinassi FA, Milton CG, Oldham JM, Hernandez P, et al. When is antipsychotic polypharmacy supported by research evidence? Implications for QI. Jt Comm J Qual Patient Saf. 2008. 34:571–582.
Article7. Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med. 1991. 151:1825–1832.
Article8. Gallagher PF, Barry PJ, Ryan C, Hartigan I, O'Mahony D. Inappropriate prescribing in an acutely ill population of elderly patients as determined by Beers' Criteria. Age Ageing. 2008. 37:96–101.
Article9. Barry PJ, O'Keefe N, O'Connor KA, O'Mahony D. Inappropriate prescribing in the elderly: a comparison of the Beers criteria and the improved prescribing in the elderly tool (IPET) in acutely ill elderly hospitalized patients. J Clin Pharm Ther. 2006. 31:617–626.
Article10. Skrbo A, Begović B, Skrbo S. [Classification of drugs using the ATC system (Anatomic, Therapeutic, Chemical Classification) and the latest changes]. Med Arh. 2004. 58:1 Suppl 2. 138–141.11. Nam JS, Shin WG, Oh JM. Pattern of medication usage and potentilly inappropriate medication among Korean ambulatory elderly patients based on an explicit criterion. Korean J Clin Pharm. 2005. 15:1–11.12. Kim MH, Kim SH. A study on factors causing the burden of medical expenses to the elderly with chronic disease. Korean J Soc Welf. 2002. 48:270–298.13. Yoo HS, Jung IK. A study on polypharmacy in the elderly psychiatric outpatients with persistent treatments for 3 years. J Korean Geriatr Psychiatry. 2010. 14:50–57.14. Mojtabai R, Olfson M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch Gen Psychiatry. 2010. 67:26–36.
Article15. Glezer A, Byatt N, Cook R Jr, Rothschild AJ. Polypharmacy prevalence rates in the treatment of unipolar depression in an outpatient clinic. J Affect Disord. 2009. 117:18–23.
Article16. Schuler J, Dückelmann C, Beindl W, Prinz E, Michalski T, Pichler M. Polypharmacy and inappropriate prescribing in elderly internal-medicine patients in Austria. Wien Klin Wochenschr. 2008. 120:733–741.
Article17. Blumstein T, Benyamini Y, Chetrit A, Mizrahi EH, Lerner-Geva L. Prevalence and correlates of psychotropic medication use among older adults in Israel: cross-sectional and longitudinal findings from two cohorts a decade apart. Aging Ment Health. 2012. 16:636–647.
Article18. Craig D, Passmore AP, Fullerton KJ, Beringer TR, Gilmore DH, Crawford VL, et al. Factors influencing prescription of CNS medications in different elderly populations. Pharmacoepidemiol Drug Saf. 2003. 12:383–387.
Article19. Peacey J, Miller H, Huthwaite MA, Romans SE. Sleep medication in acute psychiatric illness: patient's knowledge and prescription patterns in New Zealand. J Nerv Ment Dis. 2012. 200:83–87.20. Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003. 163:2716–2724.
Article21. Mundt A, Ströhle A, Heimann H, Heinz A, Grohmann R. Pharmacoepidemiology of patients hospitalized for somatoform disorders in psychiatric hospitals and departments. Pharmacoepidemiol Drug Saf. 2010. 19:687–693.
Article22. Bikowski RM, Ripsin CM, Lorraine VL. Physician-patient congruence regarding medication regimens. J Am Geriatr Soc. 2001. 49:1353–1357.
Article23. Fugh-Berman A, Ernst E. Herb-drug interactions: review and assessment of report reliability. Br J Clin Pharmacol. 2001. 52:587–595.
Article24. Yoon JL. Appropriate pharmacotherapy in elderly patients. J Korean Med Assoc. 2005. 48:24–33.
Article25. Kim BR, Song KH, An HJ, Jung GY, Shin JS. A survey on medicine use in the elderly. J Korean Gerontol Nurs. 2001. 3:208–216.26. Stahl SM. Antipsychotic polypharmacy, Part 1: Therapeutic option or dirty little secret? J Clin Psychiatry. 1999. 60:425–426.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and Predictors of Polypharmacy among Elderly Outpatients in a Public Hospital
- A Study on Polypharmacy in the Elderly Psychiatric Outpatients with Persistent Treatments for 3 years
- Factors Associated with Drug Misuse Behaviors among Polypharmacy Elderly
- Risk Factors of Potentially Inappropriate Medications and Cost by Polypharmacy among Elderly Patients of a Community Pharmacy near a Top Tier General Hospital
- Predictors of Psychiatric Outpatient Adherence after an Emergency Room Visit for a Suicide Attempt