J Korean Med Assoc.
2011 Jan;54(1):35-43.
Breast reconstruction using deep inferior epigastric artery perforator flap
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Hanyang University College of Medicine, Seoul, Korea. jtkim@hanyang.ac.kr
Abstract
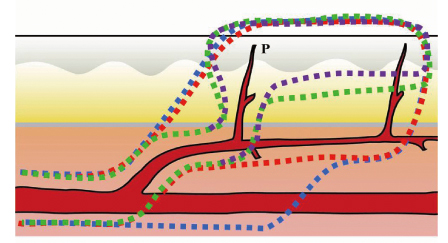
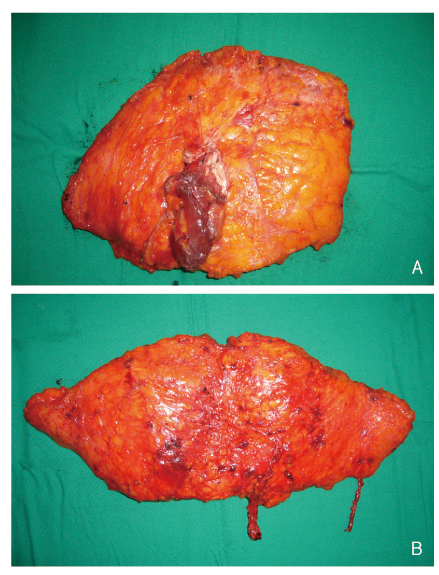
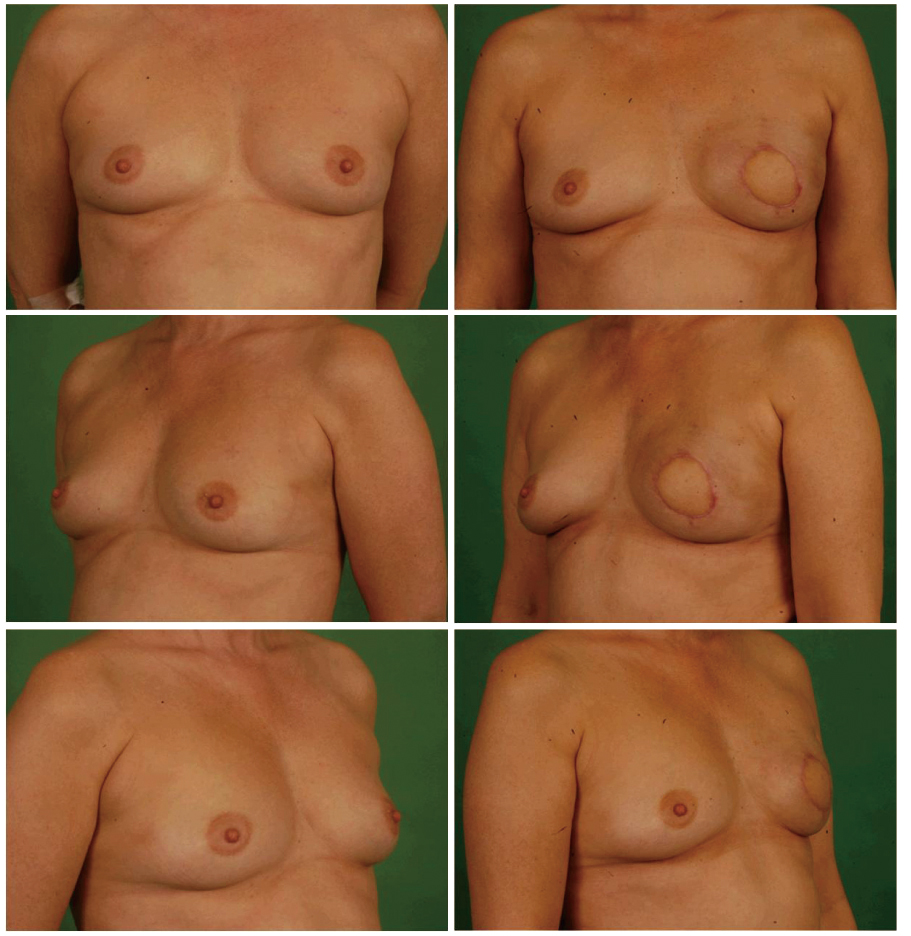
- Breast reconstruction with autologous tissue has been generally accepted as a reliable procedure, the preferred donor site being lower abdominal tissue. To sacrifice the minimal amount of muscle tissue and to reduce donor site morbidity, the concept of a perforator flap was applied to the fields of breast reconstruction, such as the deep inferior epigastric artery perforator (DIEAp) flap. The DIEAp flap provides essentially the same soft tissue components as the transverse rectus abdominis muscle (TRAM) flap while significantly reducing harvesting of the rectus muscle from the abdominal wall, thereby minimizing donor site morbidity; which includes abdominal weakness, hernia, and postoperative pain, with decreased recovery time. However, there are some concerns about the tedious and risky dissection of intramuscular perforators, and the variable vascularity of the flap supplied by tiny perforators. According to our novel flap harvesting techniques, using bipolar electrocauterization for intramuscular dissection is useful in preventing injury to the tiny perforators. Including some fibers of rectus muscle and soft tissue without full isolation and skeletonization around the pedicles is also useful for prevention of vascular injury and intraoperative vessel spasms. Moreover, the flap must include 2 to 3 reliable perforators, regardless of lateral or medial rows, for prevention of postoperative fat necrosis. The superficial inferior epigastric vein can provide additional venous drainage. These surgical tips can aid in overcoming the pitfalls of the DIEA perforator flap in breast reconstruction. The DIEAp flap is an excellent choice for breast reconstruction. According to our experience, it has been shown to be a safe and reliable method for providing good results and patient satisfaction with minimal donor morbidity in breast reconstruction.
MeSH Terms
Figure
Reference
-
1. Koshima I, Inagawa K, Urushibara K, Moriguchi T. Paraumbilical perforator flap without deep inferior epigastric vessels. Plast Reconstr Surg. 1998. 102:1052–1057.
Article2. LoTempio MM, Allen RJ. Breast reconstruction with SGAP and IGAP flaps. Plast Reconstr Surg. 2010. 126:393–401.
Article3. Chang DW, Youssef A, Cha S, Reece GP. Autologous breast reconstruction with the extended latissimus dorsi flap. Plast Reconstr Surg. 2002. 110:751–759.
Article4. Blondeel PN, Boeckx WD. Refinements in free flap breast reconstruction: the free bilateral deep inferior epigastric perforator flap anastomosed to the internal mammary artery. Br J Plast Surg. 1994. 47:495–501.
Article5. Hamdi M, Blondeel P, Van Landuyt K, Tondu T, Monstrey S. Bilateral autogenous breast reconstruction using perforator free flaps: a single center's experience. Plast Reconstr Surg. 2004. 114:83–89.
Article6. Granzow JW, Levine JL, Chiu ES, Allen RJ. Breast reconstruction with the deep inferior epigastric perforator flap: history and an update on current technique. J Plast Reconstr Aesthet Surg. 2006. 59:571–579.
Article7. Lipa JE. Breast reconstruction with free flaps from the abdominal donor site: TRAM, DIEAP, and SIEA flaps. Clin Plast Surg. 2007. 34:105–121.
Article8. Tseng CY, Lipa JE. Perforator flaps in breast reconstruction. Clin Plast Surg. 2010. 37:641–654.
Article9. Craigie JE, Allen RJ, DellaCroce FJ, Sullivan SK. Autogenous breast reconstruction with the deep inferior epigastric perforator flap. Clin Plast Surg. 2003. 30:359–369.
Article10. Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989. 42:645–648.
Article11. Kim JT. Latissimus dorsi perforator flap. Clin Plast Surg. 2003. 30:403–431.
Article12. Kim JT, Kim SK. Hand resurfacing with the superthin latissimus dorsi perforator-based free flap. Plast Reconstr Surg. 2003. 111:366–370.
Article13. Koshima I, Inagawa K, Urushibara K, Ohtsuki M, Moriguchi T. Deep inferior epigastric perforator dermal-fat or adiposal flap for correction of craniofacial contour deformities. Plast Reconstr Surg. 2000. 106:10–15.
Article14. Koshima I, Nanba Y, Tsutsui T, Takahashi Y, Watanabe A, Ishii R. Free perforator flap for the treatment of defects after resection of huge arteriovenous malformations in the head and neck regions. Ann Plast Surg. 2003. 51:194–199.
Article15. Kuo YR, Jeng SF, Wei FC, Su CY, Chien CY. Functional reconstruction of complex lip and cheek defect with free composite anterolateral thigh flap and vascularized fascia. Head Neck. 2008. 30:1001–1006.
Article16. Imai R, Matsumura H, Tanaka K, Uchida R, Watanabe K. Comparison of Doppler sonography and multidetector-row computed tomography in the imaging findings of the deep inferior epigastric perforator artery. Ann Plast Surg. 2008. 61:94–98.
Article17. Mun GH, Kim HJ, Cha MK, Kim WY. Impact of perforator mapping using multidetector-row computed tomographic angiography on free thoracodorsal artery perforator flap transfer. Plast Reconstr Surg. 2008. 122:1079–1088.
Article18. Masia J, Clavero JA, Larranaga JR, Alomar X, Pons G, Serret P. Multidetector-row computed tomography in the planning of abdominal perforator flaps. J Plast Reconstr Aesthet Surg. 2006. 59:594–599.
Article19. Mathes DW, Neligan PC. Current techniques in preoperative imaging for abdomen-based perforator flap microsurgical breast reconstruction. J Reconstr Microsurg. 2010. 26:3–10.
Article20. Hijjawi JB, Blondeel PN. Advancing deep inferior epigastric artery perforator flap breast reconstruction through multidetector row computed tomography: an evolution in preoperative imaging. J Reconstr Microsurg. 2010. 26:11–20.
Article21. Feng LJ. Recipient vessels in free-flap breast reconstruction: a study of the internal mammary and thoracodorsal vessels. Plast Reconstr Surg. 1997. 99:405–416.
Article22. Serletti JM, Moran SL, Orlando GS, Fox I. Thoracodorsal vessels as recipient vessels for the free TRAM flap in delayed breast reconstruction. Plast Reconstr Surg. 1999. 104:1649–1655.
Article23. Majumder S, Batchelor AG. Internal mammary vessels as recipients for free TRAM breast reconstruction: aesthetic and functional considerations. Br J Plast Surg. 1999. 52:286–289.
Article24. Sacks JM, Chang DW. Rib-sparing internal mammary vessel harvest for microvascular breast reconstruction in 100 consecutive cases. Plast Reconstr Surg. 2009. 123:1403–1407.
Article25. Parrett BM, Caterson SA, Tobias AM, Lee BT. The rib-sparing technique for internal mammary vessel exposure in microsurgical breast reconstruction. Ann Plast Surg. 2008. 60:241–243.
Article26. Rad AN, Flores JI, Rosson GD. Free DIEP and SIEA breast reconstruction to internal mammary intercostal perforating vessels with arterial microanastomosis using a mechanical coupling device. Microsurgery. 2008. 28:407–411.
Article27. Munhoz AM. Internal mammary perforator recipient vessels for breast reconstruction using free TRAM, DIEP, and SIEA flaps. Plast Reconstr Surg. 2008. 122:315–316.
Article28. Wu LC, Iteld L, Song DH. Supercharging the transverse rectus abdominis musculocutaneous flap: breast reconstruction for the overweight and obese population. Ann Plast Surg. 2008. 60:609–613.29. Marck KW, van der Biezen JJ, Dol JA. Internal mammary artery and vein supercharge in TRAM flap breast reconstruction. Microsurgery. 1996. 17:371–374.
Article30. Baumann DP, Lin HY, Chevray PM. Perforator number predicts fat necrosis in a prospective analysis of breast reconstruction with free TRAM, DIEP, and SIEA flaps. Plast Reconstr Surg. 2010. 125:1335–1341.
Article31. Kim JT, Kim CY, Kim YH. T-anastomosis in microsurgical free flap reconstruction: an overview of clinical applications. J Plast Reconstr Aesthet Surg. 2008. 61:1157–1163.
Article32. Kim JT, Kim YH. Initial temporary vascular insufficiency in latissimus dorsi and thoracodorsal perforator flaps. Plast Reconstr Surg. 2009. 124:6 Suppl. e408–e418.
Article33. Bailey SH, Saint-Cyr M, Wong C, Mojallal A, Zhang K, Ouyang D, Arbique G, Trussler A, Rohrich RJ. The single dominant medial row perforator DIEP flap in breast reconstruction: three-dimensional perforasome and clinical results. Plast Reconstr Surg. 2010. 126:739–751.
Article34. Schaverien MV, Perks AG, McCulley SJ. Comparison of outcomes and donor-site morbidity in unilateral free TRAM versus DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2007. 60:1219–1224.
Article35. Chen CM, Halvorson EG, Disa JJ, McCarthy C, Hu QY, Pusic AL, Cordeiro PG, Mehrara BJ. Immediate postoperative complications in DIEP versus free/muscle-sparing TRAM flaps. Plast Reconstr Surg. 2007. 120:1477–1482.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Algorithmic Approach to Total Breast Reconstruction with Free Tissue Transfer
- Deep Inferior Epigastric Perforator Flap Breast Reconstruction in a Patient with Huge Uterine Leiomyoma
- Immediate Breast Reconstruction with Deep Inferior Epigastric Perforator Free Flap
- Immediate Bilateral Breast Reconstruction with Unilateral Deep Superior Epigastric Artery and Superficial Circumflex Iliac Artery Flaps
- Simultaneous Laparoscopic Surgery during Deep Inferior Epigastric Artery Perforator Flap Elevation: A Case Report