J Korean Ophthalmol Soc.
2015 Mar;56(3):413-419. 10.3341/jkos.2015.56.3.413.
Contralateral Inferior Oblique Muscle Overaction after Unilateral Inferior Oblique Weakening Procedures
- Affiliations
-
- 1Department of Ophthalmology, Dankook University Medical College, Cheonan, Korea. kseeye@hanmail.net
- KMID: 2339048
- DOI: http://doi.org/10.3341/jkos.2015.56.3.413
Abstract
- PURPOSE
To investigate the effect of unilateral inferior oblique weakening procedures on contralateral inferior oblique muscle functions and factors that may have an effect on contralateral inferior oblique muscle overaction (IOOA).
METHODS
A retrospective chart review was conducted of medical records of 40 patients who underwent unilateral inferior oblique (IO) muscle weakening procedures from 2007 to 2011 and were observed during a follow-up period of more than 6 months. These patients were composed of primary IOOA (4 patients), secondary IOOA due to superior oblique muscle (SO) palsy (21 patients), secondary IOOA due to inferior rectus muscle palsy (1 patient), and dissociated vertical deviation (DVD) accompanied with IOOA (14 patients). Factors that may have an effect on contralateral IOOA after undergoing the operation were assessed.
RESULTS
There were 7 patients (17.5%) who had over +2 IOOA after operation. IOOA on contralateral eye was increased from average of +0.00 to average of +0.66 +/- 0.14 in 6 months after operation (p < 0.01). There were no statistically significant differences between preoperative factors and functional changes in contralateral IO muscle.
CONCLUSIONS
There were no statistical factors that may have an effect on contralateral IOOA but the possibility of masked SO palsy before performing unilateral IO weakening procedures should be considered. In patients who have unilateral DVD associated with IOOA or small hypertropia, the contralateral IOOA can be more definite after operation; thus caution should be taken before operation.
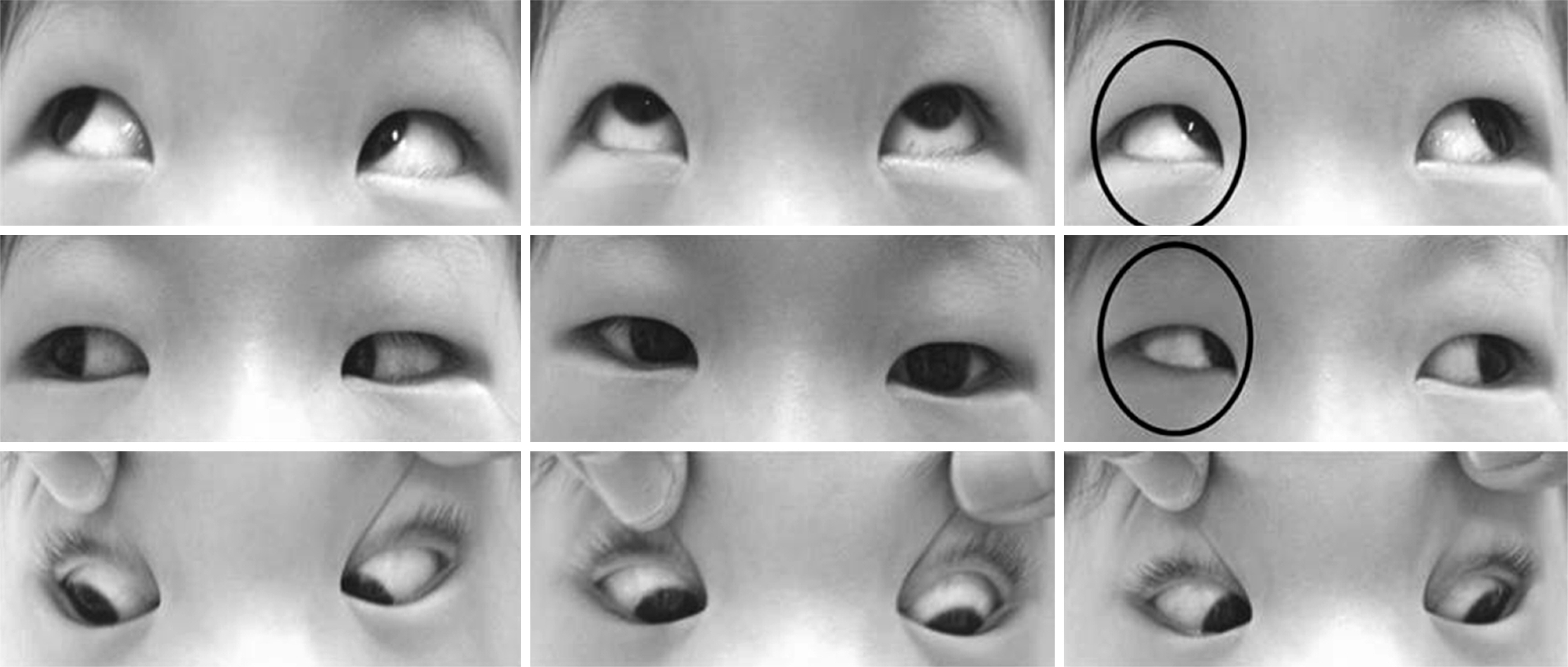
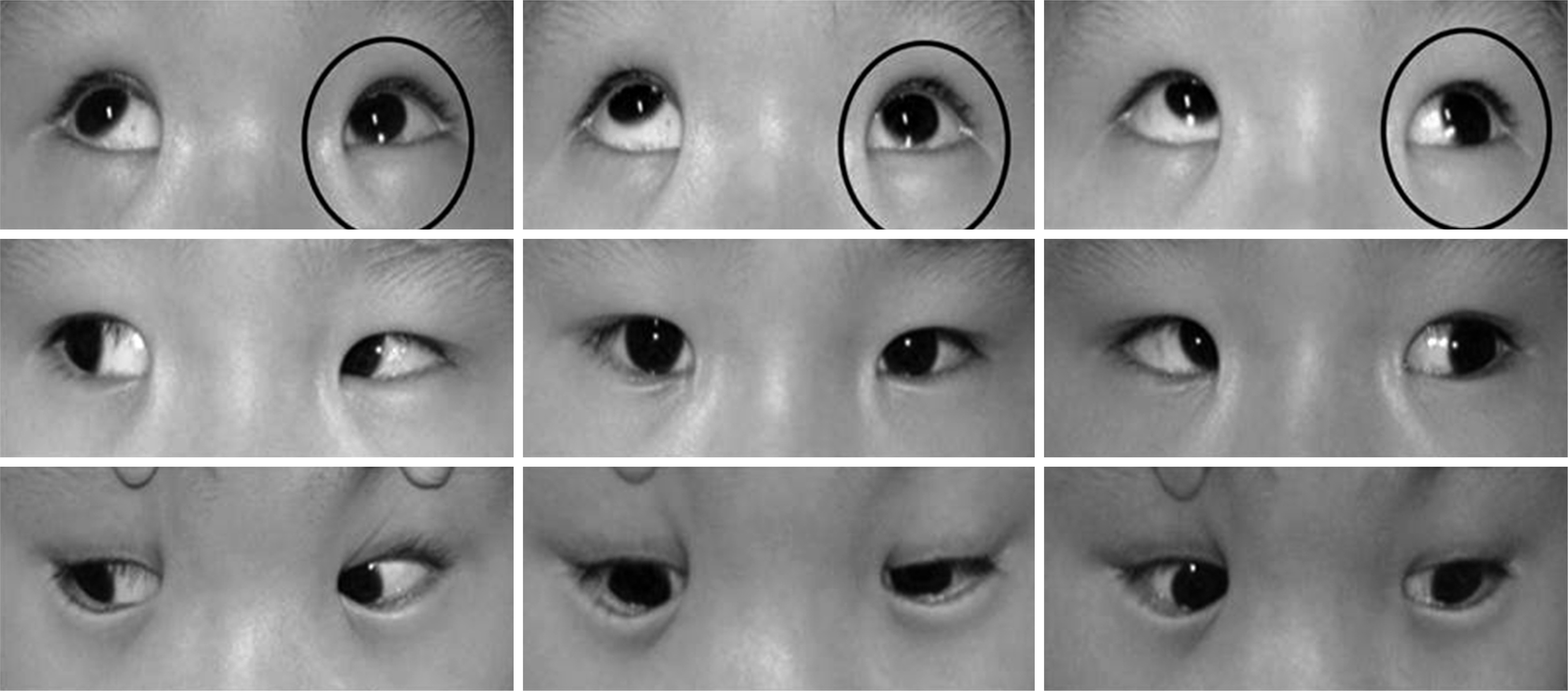
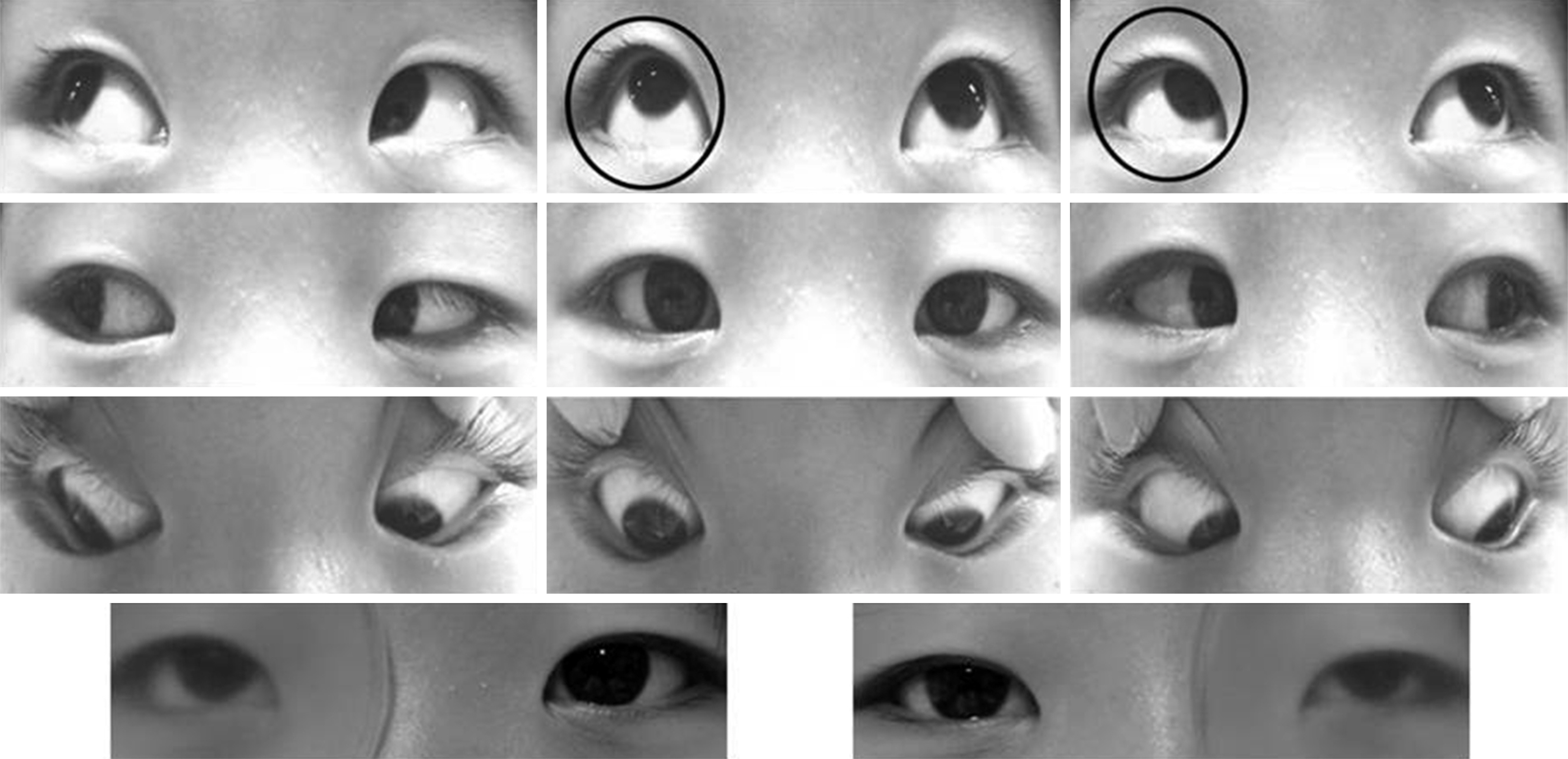
Figure
Reference
-
References
1. Parks MM, Mitchell PR. Oblique muscle dysfunctions. Tasman W, Jaeger EA, editors. Duane's clinical ophthalmology. Philadelphia: J.B. Lippincott;1994. v. 1:chap. 17.2. Wright KW. Inferior oblique surgery. Wright KW, editor. Color atlas of ophthalmic surgery, strabismus. Philadelphia: JB Lippincott;1991. p. 173–4.3. Rosenbaum AL, Santiago AP. Clinical strabismus management: principles and surgical techniques. Philadelphia: W.B. Saunders;1999. p. 449–58.4. Stein LA, Ellis FJ. Apparent contralateral inferior oblique muscle overaction after unilateral inferior oblique muscle weakening procedures. J AAPOS. 1997; 1:2–7.
Article5. Raab EL, Costenbader FD. Unilateral surgery for inferior oblique overaction. Arch Ophthalmol. 1973; 90:180–2.
Article6. Braverman DE, Scott WE. Surgical correction of dissociated vertical deviations. J Pediatr Ophthalmol. 1977; 14:337–42.
Article7. Scott WE, Sutton VJ, Thalacker JA. Superior rectus recessions for dissociated vertical deviation. Ophthalmology. 1982; 89:317–22.
Article8. Song BY, Park SW, Park YG. The surgical effects of inferior oblique anteriorization. J Korean Ophthalmol Soc. 2004; 45:995–1000.9. Ahn JH, Lee SG. Comparison of inferior oblique myectomy, recession, and anterior transposition in unilateral congenital superior oblique palsy. J Korean Ophthalmol Soc. 2010; 51:76–80.
Article10. Del Monte MA, Parks MM. Denervation and extirpation of the inferior oblique. An improved weakening procedure for marked overaction. Ophthalmology. 1983; 90:1178–85.11. von Noorden GK. Binocular vision and ocular motility: theory and management of strabismus. 5th ed.St. Louis: C.V. Mosby;1995. p. 367–8.12. Stager DR. The neurofibrovascular bundle of the inferior oblique muscle as the ancillary origin of that muscle. J AAPOS. 1997; 1:216–25.
Article13. Cho YA, Kim JH, Kim S. Antielevation syndrome after unilateral anteriorization of the inferior oblique muscle. Korean J Ophthalmol. 2006; 20:118–23.
Article14. Kim SH, Na JH, Cho YA. Inferior oblique transposition onto the equator: the role of the equator in development of contralateral inferior oblique overaction. J Pediatr Ophthalmol Strabismus. 2012; 49:98–102.
Article15. Helveston EM, Mora JS, Lipsky SN, et al. Surgical treatment of superior oblique palsy. Trans Am Ophthalmol Soc. 1996; 94:315–28. discussion 328-34.
Article16. Bielschowsky A. Lectures on motor anomalies of the eyes: II. Paralysis of individual eye muscles. Arch Ophthalmol. 1935; 13:33–59.17. Choi SW, Jung SH, Rah SH. Characteristics and outcome in horizontal strabismus combined with unilateral superior oblique palsy. J Korean Ophthalmol Soc. 2007; 48:418–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Anteriorization of The Inferior Oblique Muscle in +3 or +4 Inferior Oblique Overaction
- A Case of Contralateral Pseudo Inferior Oblique Overaction after Unilateral Inferior Oblique Anterior Transposition
- The Effect of Anterior Transposition with J-Deformity for Overaction of the Inferior Oblique Muscle
- A Study on the Anatomical Position of the Inferior Oblique Muscle Insertion in Primary Inferior Oblique Overaction
- Secondary Superior Oblique Overaction after Inferior Oblique Muscle Myectomy in a Patient Misdiagnosed with Inferior Oblique Muscle Overaction