J Korean Ophthalmol Soc.
2014 Dec;55(12):1814-1820. 10.3341/jkos.2014.55.12.1814.
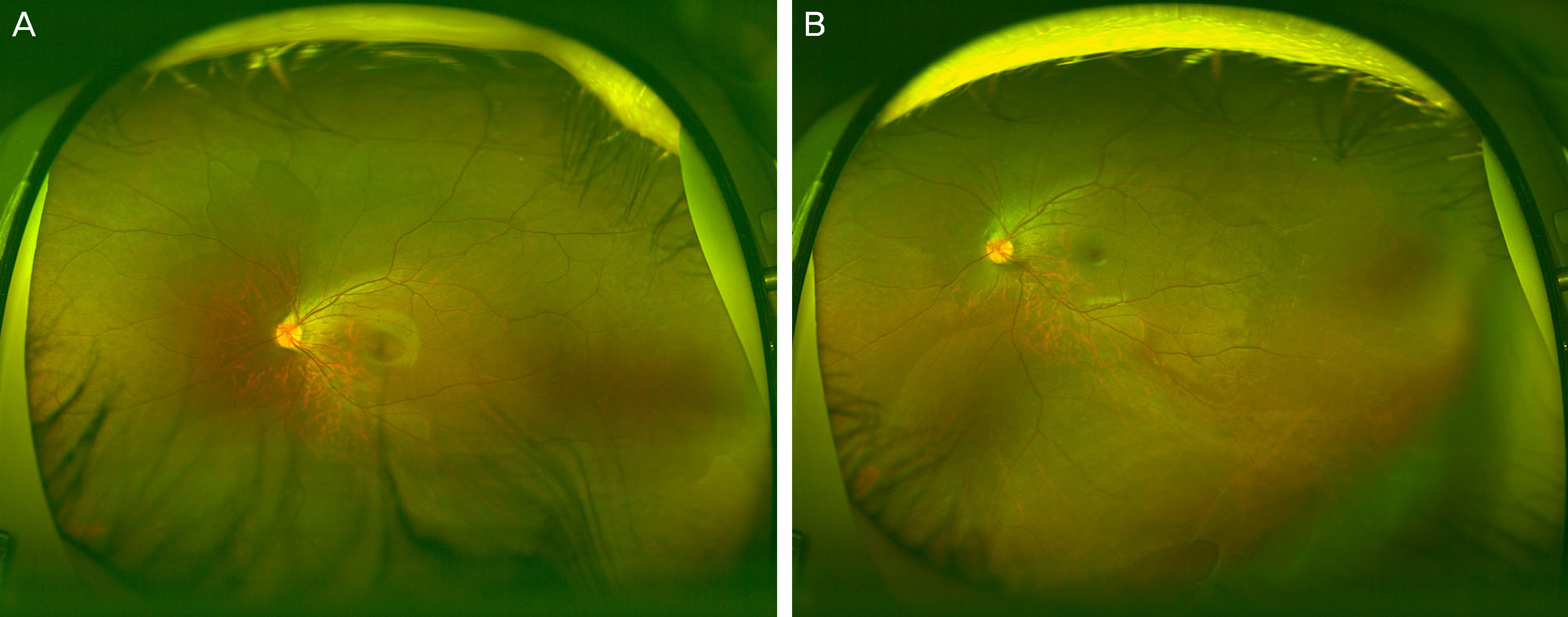
Identifiable Peripheral Retinal Lesions Using Ultra-Widefield Scanning Laser Ophthalmoscope and Its Usefulness in Myopic Patients
- Affiliations
-
- 1Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. HJKOH@yuhs.ac
- KMID: 2338966
- DOI: http://doi.org/10.3341/jkos.2014.55.12.1814
Abstract
- PURPOSE
To investigate identifiable peripheral retinal lesions in patients with myopia or high myopia and to evaluate the usefulness of ultra-widefield scanning laser ophthalmoscope in retina clinic settings.
METHODS
We evaluated fundus images of 149 patients acquired using an ultra-widefield scanning laser ophthalmoscope. Manual fundus examination by a retinal specialist was performed and sensitivity and specificity were calculated by comparing the findings of the two different fundus examination methods.
RESULTS
Variable peripheral retinal lesions were observed: lattice degeneration (24.1% in myopia, 36.6% in high myopia), white without pressure (17.7% in myopia, 20.7% in high myopia), retinal break (5.1% in myopia, 7.5% in high myopia) and retinal detachment (1.3% in myopia, 4.2% in high myopia). The incidence of lattice degeneration was significantly higher in myopic eyes than in highly myopic eyes (p = 0.043). The examination sensitivities were as follows: lattice degeneration (84.2% in myopia, 91.0% in high myopia), white without pressure (100.0% in both myopia and high myopia), retinal break (75.0% in myopia, 43.8% in high myopia) and retinal detachment (100.0% in myopia, 66.7% in high myopia). The examination specificities were 100.0% in all cases.
CONCLUSIONS
Diagnostic sensitivities of ultra-widefield scanning laser ophthalmoscope were 90.8% in patients with myopia, 91.0% in patients with high myopia and 90.9% in totally myopic patients, which were relatively high values. Therefore, the ultra- widefield scanning laser ophthalmoscope is useful as auxiliary equipment for myopic patients in retina clinic settings.
MeSH Terms
Figure
Cited by 2 articles
-
Ultra-wide Field Fundus Photography Using Eye Steering Technique in Patients with Symptomatic Posterior Vitreous Detachment
Min Han Kim, Jong-Hyun Oh
J Korean Ophthalmol Soc. 2018;59(12):1160-1165. doi: 10.3341/jkos.2018.59.12.1160.The Characteristics of Non-Retinal Lesions in the Ultra-Wide Field Scanning Laser Ophthalmoscope Image
Bo Ram Lee, Jae Moon Ahn, Jae Ryung Oh
J Korean Ophthalmol Soc. 2015;56(11):1742-1751. doi: 10.3341/jkos.2015.56.11.1742.
Reference
-
References
1. French AN, Morgan IG, Burlutsky G, et al. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013; 120:1482–91.
Article2. He M, Zeng J, Liu Y, et al. Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci. 2004; 45:793–9.
Article3. Fan DS, Lam DS, Lam RF, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004; 45:1071–5.
Article4. Pan CW, Zheng YF, Anuar AR, et al. Prevalence of refractive errors in a multiethnic Asian population: the Singapore epidemiology of eye disease study. Invest Ophthalmol Vis Sci. 2013; 54:2590–8.
Article5. Hyams SW, Neumann E. Peripheral retina in myopia. With particular reference to retinal breaks. Br J Ophthalmol. 1969; 53:300–6.
Article6. Pierro L, Camesasca FI, Mischi M, Brancato R. Peripheral retinal changes and axial myopia. Retina. 1992; 12:12–7.
Article7. Kim HW, Paik HJ, Ruh K. The relationship of axial length and peripheral retinal degeneration. J Korean Ophthalmol Soc. 1996; 37:999–1004.8. Bansal AS, Hubbard GB 3rd. Peripheral retinal findings in highly myopic children < or =10 years of age. Retina. 2010; 30(4 Suppl):S15–9.9. Lai TY, Fan DS, Lai WW, Lam DS. Peripheral and posterior pole retinal lesions in association with high myopia: a cross-sectional community-based study in Hong Kong. Eye (Lond). 2008; 22:209–13.
Article10. Chou B. Limitations of the Panoramic 200 Optomap. Optom Vis Sci. 2003; 80:671–2.
Article11. Yura T. The relationship between the types of axial elongation and the prevalence of lattice degeneration of the retina. Acta Ophthalmol Scand. 1998; 76:90–5.
Article12. Cheng SC, Yap MK, Goldschmidt E, et al. Use of the Optomap with lid retraction and its sensitivity and specificity. Clin Exp Optom. 2008; 91:373–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Characteristics of Non-Retinal Lesions in the Ultra-Wide Field Scanning Laser Ophthalmoscope Image
- Evaluation of Retinal Circulation Times in Branch Retinal Vein Occlusions with Scanning Laser Ophthalmoscope
- Peripheral Lattice Degeneration Imaging with Ultra-Widefield Swept-Source Optical Coherence Tomography
- Relationship between Optic Disc Parameters and Myopic Refractive Errors in Myopia
- Study on Retinal Circulation by Scanning Laser Ophthalmoscope I. Evaluation of Retinal Circulation Times in Non-proliferative Diabetic Retinopathy