J Korean Ophthalmol Soc.
2014 Jun;55(6):833-839.
A Study of Foveal Shape in Emmetropia and Myopia Using Spectral Domain Optical Coherence Tomography
- Affiliations
-
- 1Department of Ophthalmology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. 991027js@hanmail.net
Abstract
- PURPOSE
To investigate the shape of normal fovea in Korean subjects in their 20's using spectral domain optical coherence tomography (SD-OCT).
METHODS
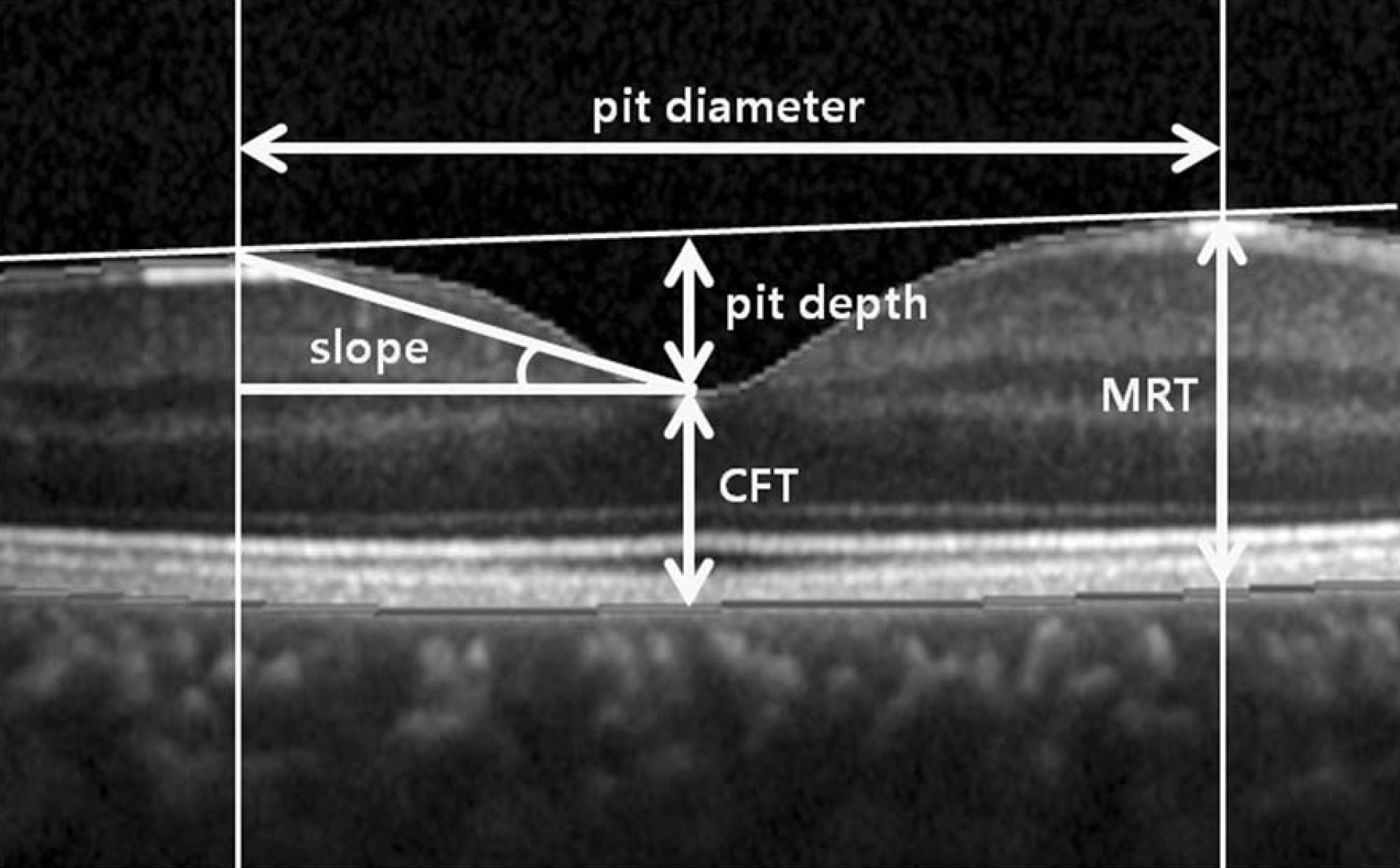
One hundred-twelve emmetropic eyes of 60 subjects and 100 myopic eyes of 58 subjects between 20 and 29 years of age were included in this study. Central foveal thickness (CFT), regional maximal retinal thickness (MRT), pit diameter, pit depth, and slope were obtained using Spectralis OCT and analyzed according to spherical equivalent and gender.
RESULTS
In emmetropic and myopic eyes, MRT was significantly thinner temporally (p < 0.001) than in other regions and pit diameter was wider horizontally than vertically (p < 0.001). The CFT was significantly thicker and all regional MRT was thinner in myopic eyes than in emmetropic eyes (p < 0.001). Foveal pits were narrower and shallower in myopic eyes (p < 0.001). In both groups, CFT and all regional MRT in males were significantly thicker than in females (p < 0.05); however, no difference between the genders in horizontal pit diameter, pit depth, and slope were found.
CONCLUSIONS
In normal subjects, statistically significant differences were found in foveal shapes between subjects with different spherical equivalent and gender. These differences should be considered when interpreting a foveal shape. Knowledge of the normal foveal morphology is important when conducting further macular studies.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Springer AD, Hendrickson AE. Development of the primate area of high acuity. 1. Use of finite element analysis models to identify mechanical variables affecting pit formation. Vis Neurosci. 2004; 21:53–62.
Article2. Springer AD, Hendrickson AE. Development of the primate area of high acuity, 3: temporal relationships between pit formation, ret-inal elongation and cone packing. Vis Neurosci. 2005; 22:171–85.
Article3. Provis JM, Diaz CM, Deher B. Ontogeny of the primate fovea: a central issue in retinal development. Prog Neurobiol. 1998; 54:549–80.4. Chen TC, Cense B, Pierce MC, et al. Spectral domain optical co-herence tomography: ultra-high speed, ultra-high resolution oph-thalmic imaging. Arch Ophthalmol. 2005; 123:1715–20.5. Moon SW, Kim ES, Kim YG, et al. The comparison of macular thickness measurements and repeatabilities between time domain and spectral domain OCT. J Korean Ophthalmol Soc. 2009; 50:1050–9.
Article6. Kang NH, Kim HJ, Lee JH. The measurements of macular thickness and volume with SD-OCT in normal eyes. J Korean Ophthalmol Soc. 2011; 52:1182–8.
Article7. Menke MN, Dabov S, Knecht P, Sturm V. Reproducibility of reti-nal thickness measurements in healthy subjects using spectralis op-tical coherence tomography. Am J Ophthalmol. 2009; 147:467–72.
Article8. Kim SH, Choi KS, Lee SJ. Macular thickness changes with age and gender in emmetropia using spectral domain optical coherence tomography. J Korean Ophthalmol Soc. 2011; 52:299–307.
Article9. Song WK, Lee SC, Lee ES, et al. Macular thickness variations with sex, age, and axial length in healthy subjects: a spectral do-main-optical coherence tomography study. Invest Ophthalmol Vis Sci. 2010; 51:3913–8.
Article10. Zou H, Zhang X, Xu X, Yu S. Quantitative in vivo retinal thickness measurement in chinese healthy subjects with retinal thickness analyzer. Invest Ophthalmol Vis Sci. 2006; 47:341–7.
Article11. Lee YJ. Analysis of factors associated with variability in measures obtained by spectral domain optical coherence tomography. J Korean Ophthalmol Soc. 2012; 53:639–46.
Article12. Wagner-Schuman M, Dubis AM, Nordgren RN, et al. Race- and sex-related differences in retinal thickness and foveal pit morphology. Invest Ophthalmol Vis Sci. 2011; 52:625–34.
Article13. Kelty PJ, Payne JF, Trivedi RH, et al. Macular thickness assessment in healthy eyes based on ethnicity using Stratus OCT optical coher-ence tomography. Invest Ophthalmol Vis Sci. 2008; 49:2668–72.
Article14. Ko BW, Shin YW, Lee JM, et al. Comparison of macular thickness measurements between Fourier-domain and Time-domain optical coherence tomography in normal eyes and eyes With macular diseases. J Korean Ophthalmol Soc. 2009; 50:1661–8.
Article15. Kim SH, Park JY, Park TK, Ohn YH. Use of spectral-domain opti-cal coherence tomography to analyze macular thickness according to refractive error. J Korean Ophthalmol Soc. 2011; 52:1286–95.
Article16. Lim MC, Hoh ST, Foster PJ, et al. Use of optical coherence tomog-raphy to assess variations in macular retinal thickness in myopia. Invest Ophthalmol Vis Sci. 2005; 46:974–8.
Article17. Lam DS, Leung KS, Mohamed S, et al. Regional variations in the relationship between macular thickness measurements and myopia. Invest Ophthalmol Vis Sci. 2007; 48:376–82.
Article18. Wu PC, Chen YJ, Chen CH, et al. Assessment of macular retinal thickness and volume in normal eyes and highly myopic eyes with third-generation optical coherence tomography. Eye (Lond). 2008; 22:551–5.
Article19. Early Treatment Diabetic Retinopathy Study Research Group. Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. ETDRS report number 7. Ophthalmology. 1991; 98:741–56.20. Tick S, Rossant F, Ghorbel I, et al. Foveal shape and structure in a normal population. Invest Ophthalmol Vis Sci. 2011; 52:5105–10.
Article21. Kumagai K, Hangai M, Larson E, Ogino N. Foveal thickness in healthy fellow eyes of patients with unilateral macular holes. Am J Ophthalmol. 2013; 156:140–8.
Article22. Ooto S, Hangai M, Sakamoto A, et al. Three-dimensional profile of macular retinal thickness in normal Japanese eyes. Invest Ophthalmol Vis Sci. 2010; 51:465–73.
Article23. Kashani AH, Zimmer-Galler IE, Shah SM, et al. Retinal thickness analysis by race, gender, and age using Stratus OCT. Am J Ophthalmol. 2010; 149:496–502.
Article24. Wakitani Y, Sasoh M, Sugimoto M, et al. Macular thickness meas-urements in healthy subjects with different axial lengths using opti-cal coherence tomography. Retina. 2003; 23:177–82.
Article25. Chan A, Duker JS, Ko TH, et al. Normal macular thickness meas-urements in healthy eyes using Stratus optical coherence tomography. Arch Ophthalmol. 2006; 124:193–8.
Article26. Kang JH, Kim SA, Song WG, Yoon HS. Macular thickness changes with age in normal subjects measured by optical coher-ence tomography. J Korean Ophthalmol Soc. 2004; 45:592–8.27. Eriksson U, Alm A. Macular thickness decreases with age in nor-mal eyes: a study on the macular thickness map protocol in the Stratus OCT. Br J Ophthalmol. 2009; 93:1448–52.
Article28. Oh SB, Cho WB, Moon JW, Kim HC. Repeatability and agreement of macular thickness measurement using time domain OCT and spectral domain OCT in normal subjects. J Korean Ophthalmol Soc. 2009; 50:710–6.
Article29. Kiernan DF, Hariprasad SM, Chin EK, et al. Prospective compar-ison of cirrus and stratus optical coherence tomography for quanti-fying retinal thickness. Am J Ophthalmol. 2009; 147:267–75.
Article30. Yanoff M, Fine BS. Ocular Pathology: A text and Atlas. 3rd ed.Philadelphia: J. B. Lippincott;1989. p. 408.31. Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004; 122:1455–60.
Article32. Coppe AM, Ripandelli G, Parisi V, et al. Prevalence of asympto-matic macular holes in highly myopic eyes. Ophthalmology. 2005; 112:2103–9.
Article33. Oie Y, Ikuno Y, Fujikado T, Tano Y. Relation of posterior staph-yloma in highly myopic eyes with macular hole and retinal detachment. Jpn J Ophthalmol. 2005; 49:530–2.
Article34. Matsumura N, Ikuno Y, Tano Y. Posterior vitreous detachment and macular hole formation in myopic foveoschisis. Am J Ophthalmol. 2004; 138:1071–3.
Article35. Yu X, Tang Y, Li F, et al. Protection against hydrogen peroxide-induced cell death in cultured human retinal pigment epithelial cells by 17beta-estradiol: a differential gene expression profile. Mech Ageing Dev. 2005; 126:1135–45.36. Evans JR, Schwartz SD, McHugh JD, et al. Systemic risk factors for idiopathic macular holes: a case-control study. Eye (Lond). 1998; 12:256–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Choroidal Thickness Variation According to Refractive Error Measured by Spectral Domain-optical Coherence Tomography in Korean Children
- Foveal Shape According to Age and Gender Using Spectral Domain Optical Coherence Tomography
- Macular Thickness Changes with Age and Gender in Emmetropia Using Spectral Domain Optical Coherence Tomography
- The Structure-function Relationships between Two Different Optical Coherence Tomography in Patients with High Myopic Glaucoma
- Use of Spectral-Domain Optical Coherence Tomography to Analyze Macular Thickness According to Refractive Error