J Korean Ophthalmol Soc.
2014 Apr;55(4):616-622.
A Case of an Isolated Abscess in an Extraocular Muscle
- Affiliations
-
- 1Department of Ophthalmology, Ewha Womans University School of Medicine, Seoul, Korea. jrmoph@ewha.ac.kr
Abstract
- PURPOSE
To report the case of an isolated abscess in an extraocular muscle.
CASE SUMMARY
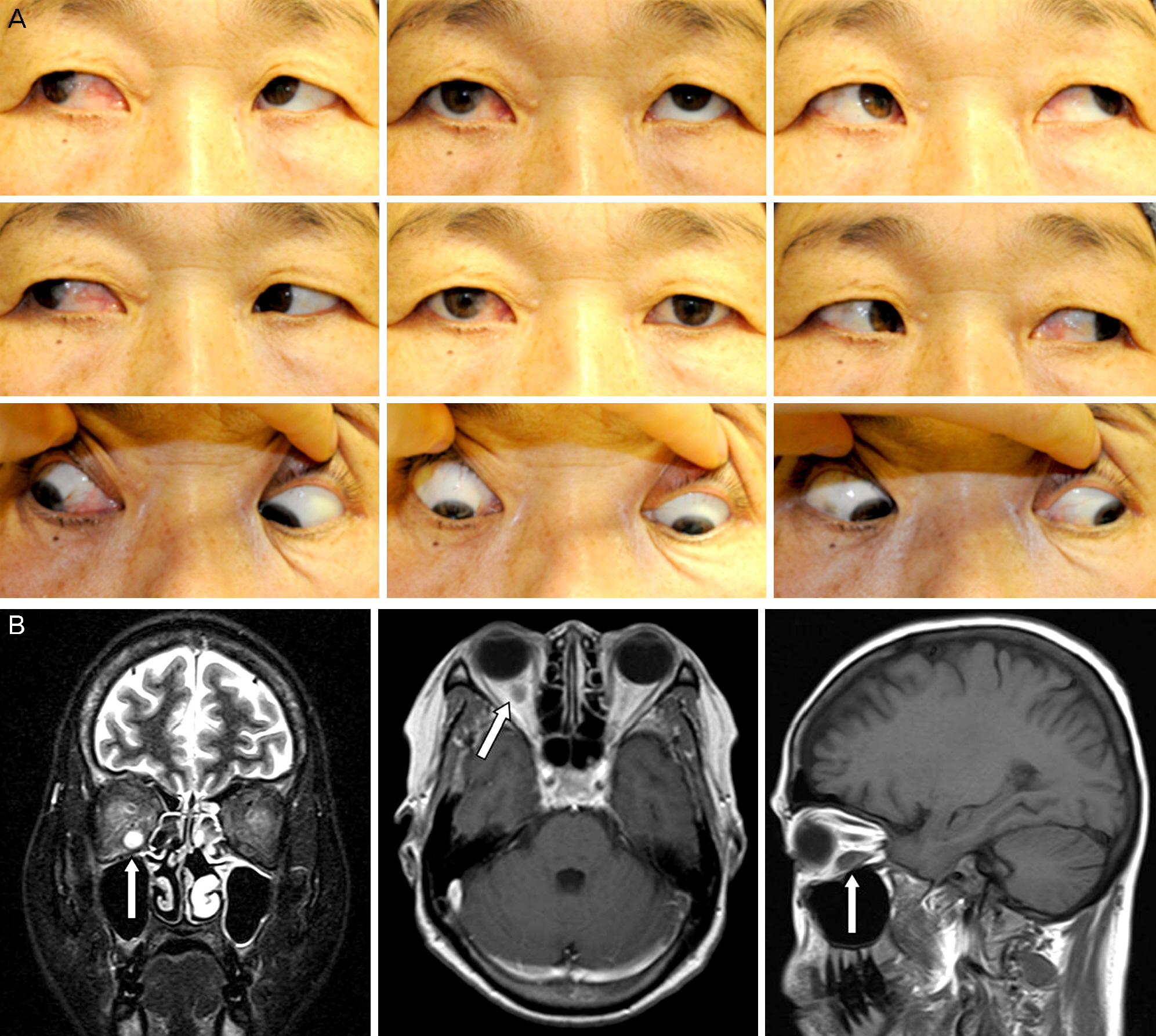
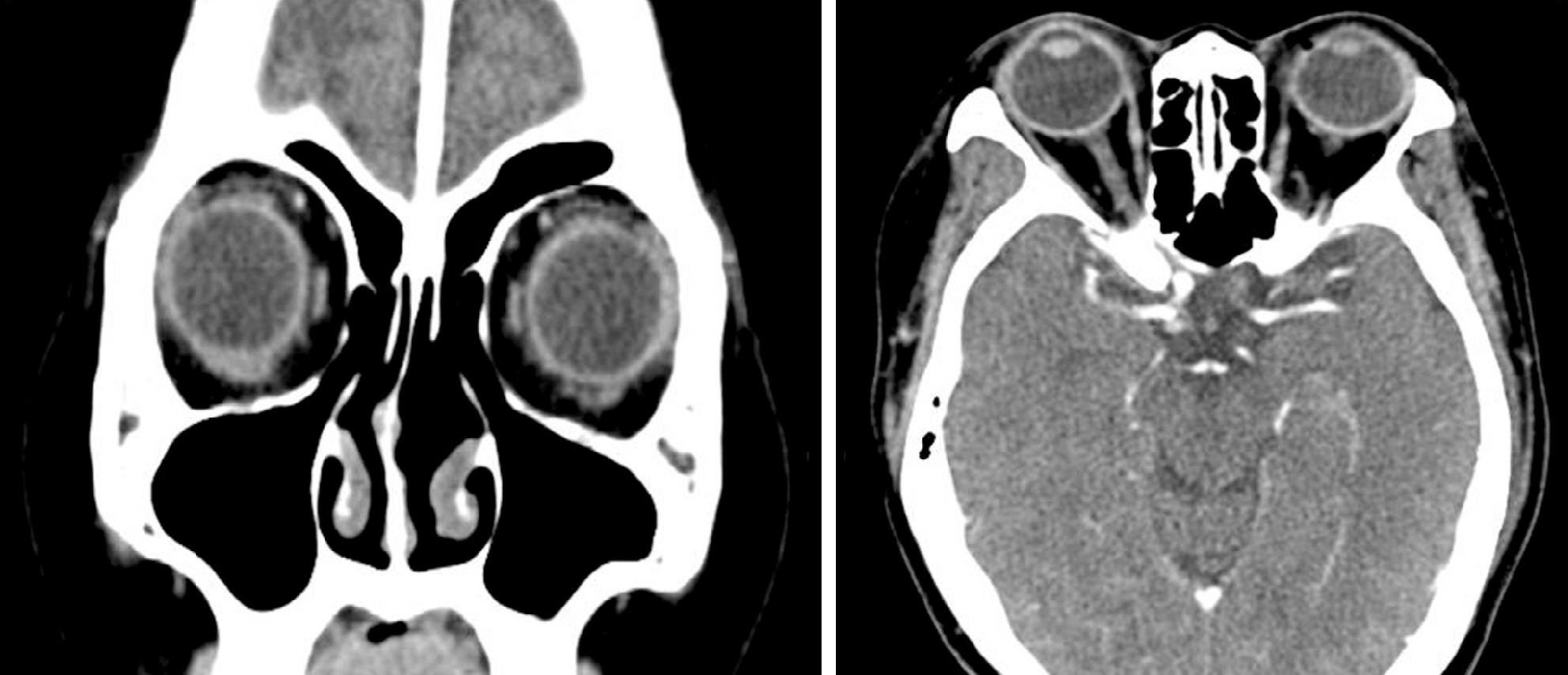
We report a case of an isolated abscess in an extraocular muscle in a patient who was treated with systemic chemotherapy for precursor B lymphoblastic leukemia. A 54-year-old female who had undergone systemic chemotherapy for precursor B lymphoblastic leukemia presented with right ocular pain and limited eye movements. On ophthalmic examination, she had elevated intraocular pressure (IOP) and limited upward and downward gaze. MRI (magnetic resonance imaging) examination revealed an isolated abscess in right inferior rectus muscle. Although the patient was treated with empirical intravenous antibiotics and IOP-lowering agents, the size of the abscess increased, as confirmed by MRI findings. Therefore, we performed a pus drainage procedure by the transconjunctival approach. We were not able to find any residual abscess lesions on CT scans 3 months postoperatively. The patient's ocular pain disappeared and the limited eye movements improved significantly 6 months postoperatively.
CONCLUSIONS
There have been no case reports of an isolated abscess in an extraocular muscle in Korea. For immunocompromised patients unresponsive to systemic empirical antibiotic treatment, an early pus drainage procedure by the transconjunctival approach may be a useful and effective therapeutic method in the management of an idiopathic isolated abscess in an extraocular muscle.
MeSH Terms
Figure
Reference
-
References
1. Sekhar GC, Lemke BN, Singh SK. Cystic lesions of the extraocular muscles. Ophthal Plast Reconstr Surg. 1996; 12:199–205.
Article2. Schramm VL Jr, Curtin HD, Kennerdell JS. Evaluation of orbital cellulitis and results of treatment. Laryngoscope. 1982; 92:732–8.
Article3. Coden DJ, Hornblass A, Haas BD. Clinical bacteriology of dacryo-cystitis in adults. Ophthal Plast Reconstr Surg. 1993; 9:125–31.
Article4. Varma A, Sharma K, Rathi B, et al. Isolated abscess of extraocular muscle in two young boys: clinical and imaging features. Orbit. 2003; 22:67–72.
Article5. Haufschild T, Weber P, Nuttli I, et al. Idiopathic isolated abscess in an extraocular muscle in a child. Arch Ophthalmol. 2004; 122:1233–4.
Article6. Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970; 80:1414–28.
Article7. Krohel GB, Krauss HR, Winnick J. Orbital abscess. Presentation, diagnosis, therapy, and sequelae. Ophthalmology. 1982; 89:492–8.8. Lee KW, Han KS. A case of orbital cellulitis complicated subdural abscess. J Korean Ophthalmol Soc. 1981; 22:475–8.9. Kaplan DM, Briscoe D, Gatot A, et al. The use of standardized orbital ultrasound in the diagnosis of sinus induced infections of the orbit in children: a preliminary report. Int J Pediatr Otorhinolaryngol. 1999; 48:155–62.
Article10. Reddy SC, Sharma HS, Mazidah AS, et al. Orbital abscess due to acute ethmoiditis in a neonate. Int J Pediatr Otorhinolaryngol. 1999; 49:81–6.
Article11. Souliere CR Jr, Antoine GA, Martin MP, et al. Selective non-surgical management of subperiosteal abscess of the orbit: compu-terized tomography and clinical course as indication for surgical drainage. Int J Pediatr Otorhinolaryngol. 1990; 19:109–19.
Article12. Tanenbaum M, Tenzell J, Byrne SF, Forster RK. Medical management of orbital abscess. Surv Ophthalmol. 1985; 30:211–2.
Article13. Sekhar GC, Lemke BN. Orbital cysticercosis. Ophthalmology. 1997; 104:1599–604.
Article14. Duke Elder S, Mc Faul PAS. System of ophthalmology. 1st ed.Vol. 13:Part II.St. Louis: CV Mosby;1974. p. 925–9.15. De Potter P, Kunin AW, Shields CL, et al. Massive orbital cyst of the lateral rectus muscle after retinal detachment surgery. Ophthal Plast Reconstr Surg. 1993; 9:292–6.16. Howard GR, Nerad JA, Bonavolonta G, Tranfa F. Orbital dermoid cysts located within the lateral rectus muscle. Ophthalmology. 1994; 101:767–71.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sinonasal Rhabdomyosarcoma Metastasis in Bilateral Multiple Extraocular Muscles: A Case Report and Brief Literature Review
- The Effects of Mg++, Ca++, Na+ and K+, on the ATPase Activity of Mitochondrial Fraction Isolated from Bovine Extraocular Muscle and Ciliary Process
- The effects of adrenergic and adrenergic blocking agents on the phosphorylase activity of bovine extraocular muscles
- Evaluation of Extraocular Muscle Contractibility after Recession and resection by EMG in Rabbit
- Isolated Unilateral Ptosis Caused by Orbital Myositis Involving the Superior Rectus-Levator Muscle