J Korean Ophthalmol Soc.
2012 Feb;53(2):283-290.
Long-Term Effects of Intravitreal Bevacizumab Injection for Macular Edema Secondary to Branch Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. maekbak@hanmail.net
Abstract
- PURPOSE
To report the long term effects of intravitreal bevacizumab injection (IVAI) for the treatment of macular edema due to branch retinal vein occlusion (BRVO).
METHODS
In this retrospective study, 47 consecutive patients (47 eyes) whose visual acuity under 20/40 and macular thickness over 250 microm from BRVO received IVAI (1.25 mg). All patients were observed over 12 months. The patients were classified into three groups: one, resolved macular edema after first injection, second, persistant, third, recurrant. At 12 months after injection, best corrected visual acuity (BCVA) and central macular thickness (CMT) were compared with one another.
RESULTS
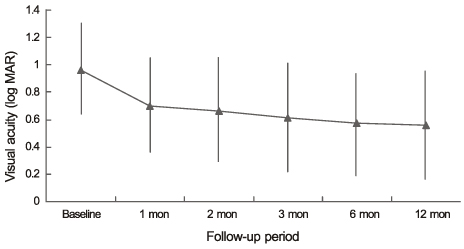
Comparing with baseline BCVA (0.96 +/- 0.32, 1.13 +/- 0.42, 0.85 +/- 0.24 log MAR unit), the mean at 12 months was significantly increased (0.50 +/- 0.30, 0.76 +/- 0.51, 0.55 +/- 0.35) in each group. The mean CMT at baseline was 510.84 (+/- 171.07), 538.5 (+/- 216.87), 522.6 (+/- 101.82) microm decreased to 211.58 (+/- 42.74), 232 (+/- 132.68), 270.6 (+/- 85.27).
CONCLUSIONS
IVAI was a result of significant decrease of CMT with improvement of BCVA in patients with BRVO after a follow-up of 12 months.
MeSH Terms
Figure
Reference
-
1. Scott IU. Vitreoretinal surgery for complications of branch retinal vein occlusion. Curr Opin Ophthalmol. 2002. 13:161–166.2. Finkelstein D, Clarkson JG. Branch Vein Occlusion Study Group. Branch and central vein occlusions. Focal Points 1987: clinical modules for ophthalmologists. Am Acad Ophthalmol. 1987. 5:1–11.3. Rehak J, Rehak M. Branch retinal vein occlusion: pathogenesis, visual prognosis, and treatment modalities. Curr Eye Res. 2008. 33:111–131.4. Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984. 98:271–282.5. Weiter JJ, Zuckerman R. The influence of photoreceptor-RPE complex on the inner retina. An explanation for the beneficial effects of photocoagulation. Ophthalmology. 1980. 87:1133–1139.6. Jonas JB, Kreissig I, Degenring R. Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br J Ophthalmol. 2003. 87:24–27.7. Jonas JB, Akkoyun I, Kamppeter B, et al. Branch retinal vein occlusion treated by intravitreal triamcinolone acetonide. Eye (Lond). 2005. 19:65–71.8. Avitabile T, Longo A, Reibaldi A. Intravitreal triamcinolone compared with macular laser grid photocoagulation for the treatment of cystoid macular edema. Am J Ophthalmol. 2005. 140:695–702.9. Cekic O, Chang S, Tseng JJ, et al. Intravitreal triamcinolone injection for treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2005. 25:851–855.10. Ozkiris A, Evereklioglu C, Erkilic K, et al. Intravitreal triamcinolone acetonide for treatment of persistent macular oedema in branch retinal vein occlusion. Eye (Lond). 2006. 20:13–17.11. Ferrara N. Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev. 2004. 25:581–611.12. Adamis AP, Shima DT. The role of vascular endothelial growth factor in ocular health and disease. Retina. 2005. 25:111–118.13. Noma H, Minamoto A, Funatsu H, et al. Intravitreal levels of vascular endothelial growth factor and interleukin-6 are correlated with macular edema in branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2006. 244:309–315.14. Pe'er J, Folberg R, Itin A, et al. Vascular endothelial growth factor upregulation in human central retinal vein occlusion. Ophthalmology. 1998. 105:412–416.15. Rabena MD, Pieramici DJ, Castellarin AA, et al. Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2007. 27:419–425.16. Spandau U, Wickenhäuser A, Rensch F, et al. Intravitreal bevacizumab for branch retinal vein occlusion. Acta Ophthalmol Scand. 2007. 85:118–119.17. Costa RA, Jorge R, Calucci D, et al. Intravitreal bevacizumab (avastin) for central and hemicentral retinal vein occlusions: IBeVO study. Retina. 2007. 27:141–149.18. Wu L, Arevalo JF, Roca JA, et al. Comparison of two doses of intravitreal bevacizumab (Avastin) for treatment of macular edema secondary to branch retinal vein occlusion: results from the Pan-American Collaborative Retina Study Group at 6 months of follow-up. Retina. 2008. 28:212–219.19. Kriechbaum K, Michels S, Prager F, et al. Intravitreal Avastin for macular oedema secondary to retinal vein occlusion: a prospective study. Br J Ophthalmol. 2008. 92:518–522.20. Kreutzer TC, Alge CS, Wolf AH, et al. Intravitreal bevacizumab for the treatment of macular oedema secondary to branch retinal vein occlusion. Br J Ophthalmol. 2008. 92:351–355.21. Jaissle GB, Leitritz M, Gelisken F, et al. One-year results after intravitreal bevacizumab therapy for macular edema secondary to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2009. 247:27–33.22. Prager F, Michels S, Kriechbaum K, et al. Intravitreal bevacizumab (Avastin) for macular oedema secondary to retinal vein occlusion: 12-month results of a prospective clinical trial. Br J Ophthalmol. 2009. 93:452–456.23. Kondo M, Kondo N, Ito Y, et al. Intravitreal injection of bevacizumab for macular edema secondary to branch retinal vein occlusion: results after 12 months and multiple regression analysis. Retina. 2009. 29:1242–1248.24. Chung EJ, Hong YT, Lee SC, et al. Prognostic factors for visual outcome after intravitreal bevacizumab for macular edema due to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2008. 246:1241–1247.25. Klein R, Klein BE, Moss SE, et al. The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc. 2000. 98:133–141.26. Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion in Australia. The Blue Mountains Eye Study. Arch Ophthalmol. 1996. 114:1243–1247.27. David R, Zangwill L, Badarna M, Yassur Y. Epidemiology of retinal vein occlusion and its association with glaucoma and increased intraocular pressure. Ophthalmologica. 1988. 197:69–74.28. Gutman FA, Zegarra H. The natural course of temporal retinal branch vein occlusion. Trans Am Acad Ophthalmol Otolaryngol. 1974. 78:OP178–OP192.29. Hayreh SS, Rojas P, Podhajsky P, et al. Ocular neovascularization with retinal vascular occlusion-III. Incidence of ocular neovascularization with retinal vein occlusion. Ophthalmology. 1983. 90:488–506.30. Magargal LE, Kimmel AS, Sanborn GE, et al. Temporal branch retinal vein obstruction: a review. Ophthalmic Surg. 1986. 17:240–246.31. Michels RG, Gass JDM. Natural course of temporal retinal branch occlusion. Trans Am Acad Ophthalmol Otolaryngol. 1974. 78:178–192.32. Stefánsson E. The therapeutic effects of retinal laser treatment and vitrectomy. A theory based on oxygen and vascular physiology. Acta Ophthalmol Scand. 2001. 79:435–440.33. Kalogeropoulos C, Donati G, Pizzolato GP, Pournaras CJ. Morphology of early retinal lesions after experimental venous occlusion. Klin Monbl Augenheilkd. 1996. 208:375–376.34. Larsson J, Bauer B, Andréasson S. The 30-Hz flicker cone ERG for monitoring the early course of central retinal vein occlusion. Acta Ophthalmol Scand. 2000. 78:187–190.35. Rabena MD, Pieramici DJ, Castellarin AA, et al. Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2007. 27:419–425.36. Matsumoto Y, Freund KB, Peiretti E, et al. Rebound macular edema following bevacizumab (Avastin) therapy for retinal venous occlusive disease. Retina. 2007. 27:426–431.37. Campochiaro PA, Hafiz G, Shah SM, et al. Ranibizumab for macular edema due to retinal vein occlusions: implication of VEGF as a critical stimulator. Mol Ther. 2008. 16:791–799.38. Jaissle GB, Ziemssen F, Petermeier K, et al. Bevacizumab for treatment of macular edema secondary to retinal vein occlusion. Ophthalmologe. 2006. 103:471–475.39. Ahmadieh H, Moradian S, Malihi M. Rapid regression of extensive retinovitreal neovascularization secondary to branch retinal vein occlusion after a single intravitreal injection of bevacizumab. Int Ophthalmol. 2005. 26:191–193.40. Yazdani S, Hendi K, Pakravan M. Intravitreal bevacizumab (Avastin) injection for neovascular glaucoma. J Glaucoma. 2007. 16:437–439.41. Kahook MY, Schuman JS, Noecker RJ. Intravitreal bevacizumab in a patient with neovascular glaucoma. Ophthalmic Surg Lasers Imaging. 2006. 37:144–146.42. Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010. 117:1102–1112.43. Lee HK, Kim HW, Yun IH. Intravitreal bevacizumab injection for macular edema secondary to branch retinal vein occlusion. J Korean Ophthalmol Soc. 2009. 50:1800–1808.44. Wetzig PC. The treatment of acute branch vein occlusion by photocoagulation. Am J Ophthalmol. 1979. 87:65–73.45. Krohne TU, Eter N, Holz FG, et al. Intraocular pharmacokinetics of bevacizumab after a single intravitreal injection in humans. Am J Ophthalmol. 2008. 146:508–512.46. Stewart MW. Predicted biologic activity of intravitreal bevacizumab. Retina. 2007. 27:1196–1200.47. Ach T, Hoeh AE, Schaal KB, et al. Predictive factors for changes in macular edema in intravitreal bevacizumab therapy of retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2010. 248:155–159.48. Lang GE, Händel A. Results of laser coagulation of retinal branch vein occlusion. Klin Monatsbl Augenheilkd. 1993. 203:180–188.49. Shilling JS, Jones CA. Retinal branch vein occlusion: a study of argon laser photocoagulation in the treatment of macular oedema. Br J Ophthalmol. 1984. 68:196–198.50. Duff IF, Falls HF, Linman JW. Anticoagulant therapy in occlusive vascular disease of retina. AMA Arch Ophthalmol. 1951. 46:601–617.51. Shroff D, Mehta DK, Arora R, et al. Natural history of macular status in recent-onset branch retinal vein occlusion: an optical coherence tomography study. Int Ophthalmol. 2008. 28:261–268.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravitreal Bevacizumab Injection for Macular Edema Secondary to Branch Retinal Vein Occlusion: Long-Term Results
- Effects of Intravitreal Bevacizumab Injection in 3 Types of Macular Edema Secondary to Branch Retinal Vein Occlusion
- Short-term Effects of Intravitreal Bevacizumab Injection and Macular Edema Patterns in Branch Retinal Vein Occlusion
- The Efficacy of Intravitreal Bevacizumab in the Treatment of Macular Edema
- Intravitreal Bevacizumab Injection for Macular Edema Secondary to Branch Retinal Vein Occlusion