J Korean Orthop Assoc.
2011 Dec;46(6):507-511.
Simple Subperiosteal Hematoma with a Periosteal Reaction Mimicking a Malignancy
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. hyunsd@cnu.ac.kr
- 2Department of Orthopedic Surgery, Dong-A University School of Medicine, Busan, Korea.
Abstract
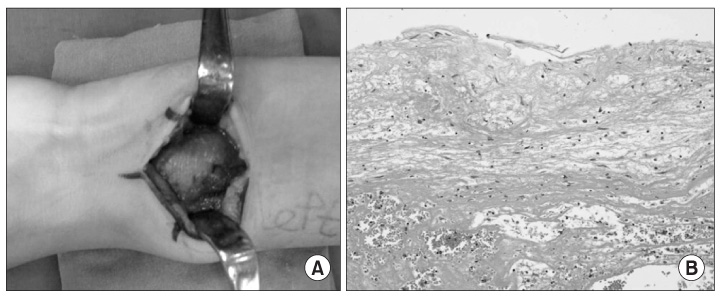
- A benign periosteal reaction, which can occur after trauma or stress, has a solid and uninterrupted appearance on radiography. In contrast, an aggressive periosteal reaction, which may indicate a malignancy, appears as a Codman's triangle or with a spiculated and sunburst pattern. In the present case, an 11-year-old boy with a previous injury to the distal radial growth plate presented with diffuse osteolysis on the distal radial metaphysis and decreased opacity of the lateral side cortex on plain radiograph. A Codman's triangle-like lesion was seen on the lateral side of the distal radius, and a few spicules were observed on the medial side of the distal radius. A T2-weighted coronal magnetic resonance image revealed a mass that had stripped the periosteum; the mass had heterogeneous signal intensity and a fl uid-fluid level on axial views. The margins of the mass were unclear, but enhanced. Suspecting a primary malignancy, we performed a biopsy. The pathology revealed that the mass was a simple hematoma.
Keyword
MeSH Terms
Figure
Reference
-
1. Miller TT. Bone tumors and tumorlike conditions: analysis with conventional radiography. Radiology. 2008. 246:662–674.
Article2. Ragsdale BD, Madewell JE, Sweet DE. Radiologic and pathologic analysis of solitary bone lesions. Part II: periosteal reactions. Radiol Clin North Am. 1981. 19:749–783.3. Koskinen SK, Mattila KT, Alanen AM, Aro HT. Stress fracture of the ulnar diaphysis in a recreational golfer. Clin J Sport Med. 1997. 7:63–65.
Article4. Ward WG Sr, Sekiya JK, Pope TL Jr. Traumatic ossifying periostitis of the ulna masquerading as a malignancy in a football player. A case report and literature review. Am J Sports Med. 1996. 24:852–856.5. Song KS, Kim HG, Park BM, Kim JM, Jung SH, Yang BS. Post traumatic osteolysis of the pubic bone simulating malignancy or osteomyelitis - a case report -. J Korean Bone Joint Tumor Soc. 2007. 13:180–184.6. Jahng J, Kim YH, Lee KS. Tuberculosis of the lower lumbar spine with an atypical radiological presentation -a case mimicking a malignancy-. Asian Spine J. 2007. 1:102–105.7. Shopfner CE. Periosteal bone growth in normal infants. A preliminary report. Am J Roentgenol Radium Ther Nucl Med. 1966. 97:154–163.8. Wenaden AE, Szyszko TA, Saifuddin A. Imaging of periosteal reactions associated with focal lesions of bone. Clin Radiol. 2005. 60:439–456.
Article9. Ishibashi Y, Okamura Y, Otsuka H, Nishizawa K, Sasaki T, Toh S. Comparison of scintigraphy and magnetic resonance imaging for stress injuries of bone. Clin J Sport Med. 2002. 12:79–84.
Article10. Resnick D. Diagnosis of bone and joint disorders. 2002. 4th ed. Philadelphia: WB Saunders;2346–2373.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Periosteal Reaction of Osteomyelitis: MRI Findings Compared with Plain Radiographs
- Exophthalmos Caused by Subperiosteal Orbital Hematoma
- Subperiosteal hematoma of the orbit associated with sinusitis
- A Case of Subperiosteal Orbital Hematoma in Patient with Ethmoid and Maxillary Sinusitis
- A Case of Subperiosteal Orbital Hematoma Associated with von Willebrand Disease