J Korean Orthop Assoc.
2011 Oct;46(5):380-386.
Clinical Results after a Rehabilitation Program for Lateral Epicondylitis of the Elbow
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Paik Hospital, College of Medicine, Inje University, Seoul, Korea.
- 2Department of Orthopedic Surgery, Green Hospital, Seoul, Korea. shinabro2000@hanmail.net
Abstract
- PURPOSE
The purpose of this study is to evaluate the clinical effectiveness of a rehabilitation program for the patients with lateral epicondylitis.
MATERIALS AND METHODS
Twenty-three patients with lateral epicondylitis were included from April 2009 to October 2009 and all the patients were treated with a rehabilitation program for 6 weeks. The evaluation at baseline and at 12 weeks after rehabilitation included the subjective assessment of symptoms and the objective assessment with measuring the grip strength and muscle power of the wrist extensors and flexors and the forearm supinators and pronators. After 6 months, subjective satisfaction was evaluated via telephone calls. The data was analyzed using the Wilcoxon signed rank test (SPSS ver. 16.0).
RESULTS
At 12 weeks, the subjective satisfaction was improved in on the three questionnaires. The grip strength increased from 25.1 kg to 37.8 kg (p<0.05). On the Biodex analysis, there was significant difference at the wrist extensors. At 6 months, 21 cases had excellent or good results according to the score and 2 cases complained of remaining pain.
CONCLUSION
Our rehabilitation program is thought to be good treatment for the patients with lateral epicondylitis, and it is a practical and precautionary step for the cases of lateral epicondylitis if the patients themselves are educated to volutarily participate in the program.
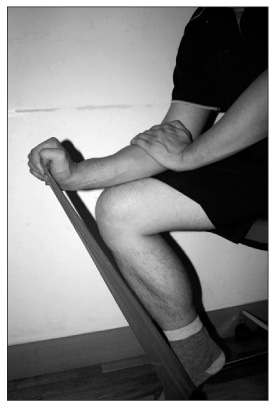
Figure
Reference
-
1. Labelle H, Guibert R, Joncas J, Newman N, Fallaha M, Rivard CH. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow. An attempted meta-analysis. J Bone Joint Surg Br. 1992. 74:646–651.
Article2. Smidt N, Assendelft WJ, Arola H, et al. Effectiveness of physiotherapy for lateral epicondylitis: a systematic review. Ann Med. 2003. 35:51–62.
Article3. Hume PA, Reid D, Edwards T. Epicondylar injury in sport: epidemiology, type, mechanisms, assessment, management and prevention. Sports Med. 2006. 36:151–170.4. Ellenbecker TS, Reinold M, Nelson CO. Clinical concepts for treatment of the elbow in the adolescent overhead athlete. Clin Sports Med. 2010. 29:705–724.
Article5. Kibler WB, Chandler TJ. Fu FH, Stone DA, editors. Racquet sports. Sports injuries: mechanism, prevention, and treatment. 1994. Baltimore: Williams & Wilkins;278–292.6. Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999. 81:259–278.7. Jensen K, Di Fabio RP. Evaluation of eccentric exercise in treatment of patellar tendinitis. Phys Ther. 1989. 69:211–216.
Article8. Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res. 1986. 208:65–68.
Article9. Fyfe I, Stanish WD. The use of eccentric training and stretching in the treatment and prevention of tendon injuries. Clin Sports Med. 1992. 11:601–624.
Article10. Svernlöv B, Adolfsson L. Non-operative treatment regime including eccentric training for lateral humeral epicondylalgia. Scand J Med Sci Sports. 2001. 11:328–334.
Article11. Martinez-Silvestrini JA, Newcomer KL, Gay RE, Schaefer MP, Kortebein P, Arendt KW. Chronic lateral epicondylitis: comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening. J Hand Ther. 2005. 18:411–419.
Article12. Stasinopoulos D, Stasinopoulou K, Johnson MI. An exercise programme for the management of lateral elbow tendinopathy. Br J Sports Med. 2005. 39:944–947.
Article13. Croisier JL, Foidart-Dessalle M, Tinant F, Crielaard JM, Forthomme B. An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopathy. Br J Sports Med. 2007. 41:269–275.
Article14. Finestone HM, Rabinovitch DL. Tennis elbow no more: practical eccentric and concentric exercises to heal the pain. Can Fam Physician. 2008. 54:1115–1116.15. DeLee JC. Leadbetter WB, Buckwalter JA, Gordon SL, editors. Tissue remodeling and response to therapeutic exercise. Sports-induced inflammation: clinical and basic science concepts. 1990. Park Ridge, IL: AAOS;547–554.16. Tipton CM, Matthes RD, Maynard JA, Carey RA. The influence of physical activity on ligaments and tendons. Med Sci Sports. 1975. 7:165–175.
Article17. Alfredson H. Chronic midportion Achilles tendinopathy: an update on research and treatment. Clin Sports Med. 2003. 22:727–741.
Article18. Ohberg L, Alfredson H. Effects on neovascularisation behind the good results with eccentric training in chronic midportion Achilles tendinosis? Knee Surg Sports Traumatol Arthrosc. 2004. 12:465–470.
Article19. Kibler WB. Clinical implications of exercise: injury and performance. Instr Course Lect. 1994. 43:17–24.20. Haahr JP, Andersen JH. Physical and psychosocial risk factors for lateral epicondylitis: a population based case-referent study. Occup Environ Med. 2003. 60:322–329.
Article21. Nilsson P, Thom E, Baigi A, Marklund B, Månsson J. A prospective pilot study of a multidisciplinary home training programme for lateral epicondylitis. Musculoskeletal Care. 2007. 5:36–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonographic Findings of Common Pathologic Conditions of the Elbow and Injections Focusing on Lateral Epicondylitis
- Lateral Epicondylitis: Current Concept
- The Effect of Prolotherapy on Lateral Epicondylitis of Elbow
- Arthroscopic Treatment for Lateral Epicondylitis of the Elbow
- Shockwave Therapy for Tennis Elbow