J Korean Assoc Oral Maxillofac Surg.
2015 Feb;41(1):52-56. 10.5125/jkaoms.2015.41.1.52.
An unusual abscess formation in the masticator space after acupressure massage: a case report
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. OMS_kspark@paik.ac.kr
- KMID: 2328655
- DOI: http://doi.org/10.5125/jkaoms.2015.41.1.52
Abstract
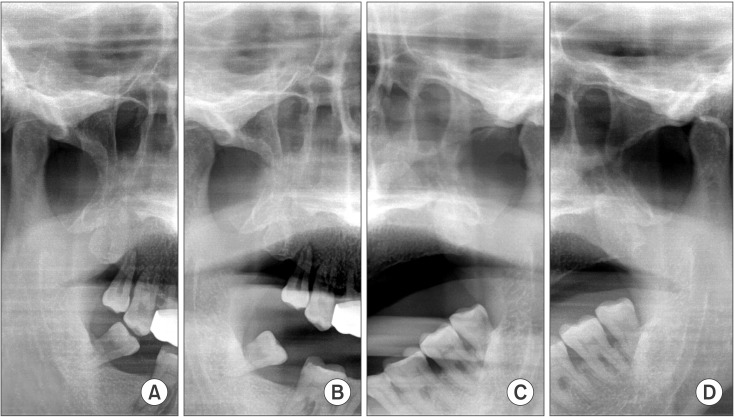
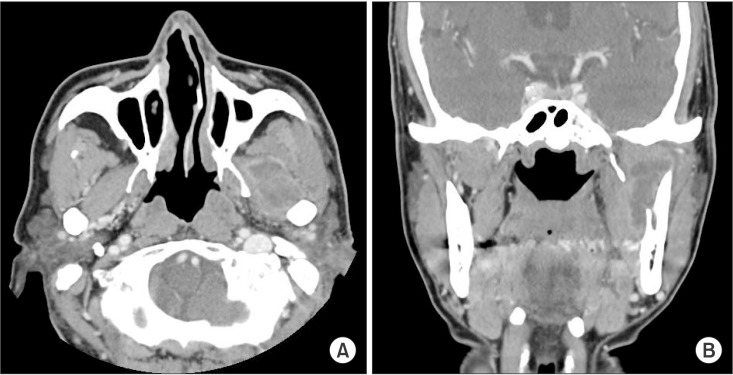
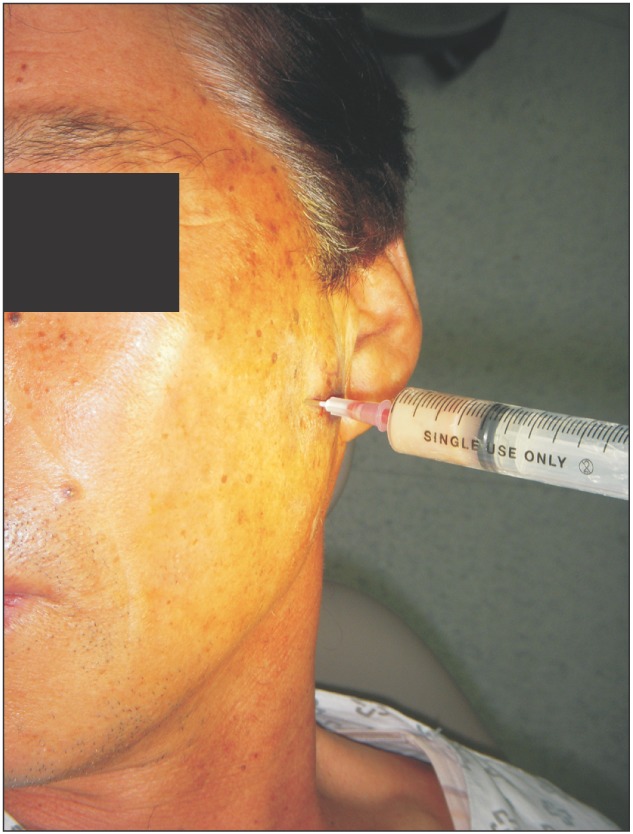
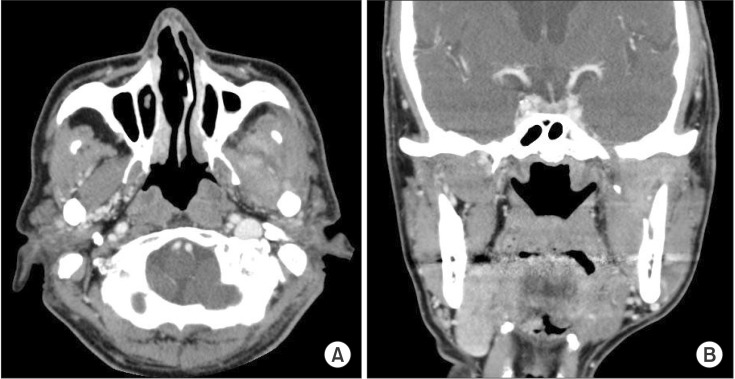
- Clinical features of masticator-space abscess (MSA) are very similar to those of parotitis or temporomandibular disorder (TMD), making early differential diagnosis difficult. Local causes of MSA include nerve block anesthesia, infection after tooth extraction, and trauma to the temporomandibular joint (TMJ); the systemic cause is immunodeficiency. Odontogenic causes account for most etiologies, but there are also unusual causes of MSA. A 66-year-old male patient visited the emergency room (ER) presenting with left-side TMJ pain three days after receiving an acupressure massage. He was tentatively diagnosed with conventional post-trauma TMD and discharged with medication. However, the patient returned to the ER with increased pain. At this time, his TMD diagnosis was confirmed. He made a third visit to the ER during which facial computed tomographic (CT) images were taken. CT readings identified an abscess or hematoma in the left masticator space. After hospitalizing the patient, needle aspiration confirmed pus in the infratemporal and temporal fossa. Antibiotics were administered, and the abscess was drained through an incision made by the attending physician. The patient's symptoms decreased, and he was discharged.
MeSH Terms
Figure
Reference
-
1. Curtin HD. Separation of the masticator space from the parapharyngeal space. Radiology. 1987; 163:195–204. PMID: 3823435.
Article2. Chong VF, Fan YF. Pictorial review: radiology of the masticator space. Clin Radiol. 1996; 51:457–465. PMID: 8689819.
Article3. Hasegawa T, Shibuya Y, Kuroki S, Takeuchi J, Yokoo S, Umeda M, et al. Two cases of masticator space abscess initially diagnosed as temporomandibular joint disorder. Kobe J Med Sci. 2008; 54:E163–E168. PMID: 19246964.4. Kamath MP, Bhojwani KM, Mahale A, Meyyappan H, Abhijit K. Infratemporal fossa abscess: a diagnostic dilemma. Ear Nose Throat J. 2009; 88:E23. PMID: 19444778.5. Raghava N, Evans K, Basu S. Infratemporal fossa abscess: complication of maxillary sinusitis. J Laryngol Otol. 2004; 118:377–378. PMID: 15165316.
Article6. Weiss BR. Infratemporal fossa abscess unusual complication of maxillary sinus fracture. Laryngoscope. 1977; 87:1130–1133. PMID: 875575.
Article7. Connor SE, Davitt SM. Masticator space masses and pseudomasses. Clin Radiol. 2004; 59:237–245. PMID: 15037135.
Article8. Chossegros C, Cheynet F, Conrath J. Infratemporal space infection after temporomandibular arthroscopy: an unusual complication. J Oral Maxillofac Surg. 1995; 53:949–951. PMID: 7629629.9. Kim HM, Kim TW, Hwang JH, Lee DJ, Park NR, Song SI. Infection of the temporomandibular joint: a report of three cases. J Korean Assoc Oral Maxillofac Surg. 2011; 37:510–514.
Article10. Morrison A, Brady J. Temporal space abscess secondary to mandibular dental extraction. Oral Health. 2009; 99:17–21.11. Matsumura Y, Inui M, Tagawa T. Peritemporomandibular abscess as a complication of acupuncture: a case report. J Oral Maxillofac Surg. 1998; 56:495–496. PMID: 9541352.
Article12. Goldschmidt MJ, Butterfield KJ, Goracy ES, Goldberg MH. Streptococcal infection of the temporomandibular joint of hematogenous origin: a case report and contemporary therapy. J Oral Maxillofac Surg. 2002; 60:1347–1353. PMID: 12420272.
Article13. Bounds GA, Hopkins R, Sugar A. Septic arthritis of the temporomandibular joint--a problematic diagnosis. Br J Oral Maxillofac Surg. 1987; 25:61–67. PMID: 2948546.
Article14. Hardin CW, Harnsberger HR, Osborn AG, Doxey GP, Davis RK, Nyberg DA. Infection and tumor of the masticator space: CT evaluation. Radiology. 1985; 157:413–417. PMID: 4048449.
Article15. Esterhai JL Jr, Gelb I. Adult septic arthritis. Orthop Clin North Am. 1991; 22:503–514. PMID: 1852426.
Article16. Gossling J. Occurrence and pathogenicity of the Streptococcus milleri group. Rev Infect Dis. 1988; 10:257–285. PMID: 3287560.
Article17. Whiley RA, Fraser H, Hardie JM, Beighton D. Phenotypic differentiation of Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus strains within the "Streptococcus milleri group". J Clin Microbiol. 1990; 28:1497–1501. PMID: 2380375.
Article18. Jacobs JA, Pietersen HG, Stobberingh EE, Soeters PB. Streptococcus anginosus, Streptococcus constellatus and Streptococcus intermedius. Clinical relevance, hemolytic and serologic characteristics. Am J Clin Pathol. 1995; 104:547–553. PMID: 7572815.
Article19. Claridge JE 3rd, Attorri S, Musher DM, Hebert J, Dunbar S. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus ("Streptococcus milleri group") are of different clinical importance and are not equally associated with abscess. Clin Infect Dis. 2001; 32:1511–1515. PMID: 11317256.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wernicke's encephalopathy in a patient with masticator and parapharyngeal space abscess: a case report
- Masticator space abscess in a 47-day-old infant
- MR Imaging of Masticator Space Infection
- Effect of Acupressure Massage on Temperatures of Acupoints, Severity of Facial Paralysis, Subjective Symptoms, and Depression in Bell's Palsy Patients
- Masticator Space Lesions: MRI and CT Findings