J Korean Assoc Oral Maxillofac Surg.
2013 Oct;39(5):231-237.
Evaluation of Korean teenagers with temporomandibular joint disorders
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Department of Oral and Maxillofacial Surgery, School of Dentistry, Chosun University, Gwangju, Korea. sgckim@chosun.ac.kr
Abstract
OBJECTIVES
This study aims to evaluate the severity and pattern of symptoms exhibited by teenage Korean temporomandibular disorder (TMD) patients.
MATERIALS AND METHODS
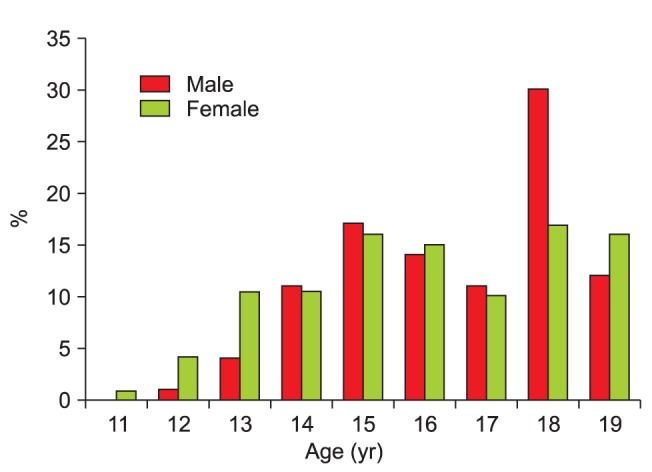
Among patients with an association of TMDs, teenage patients (11-19 years) who answered the questionnaire on the research diagnostic criteria for TMD (RDC/TMD) were recruited.
RESULTS
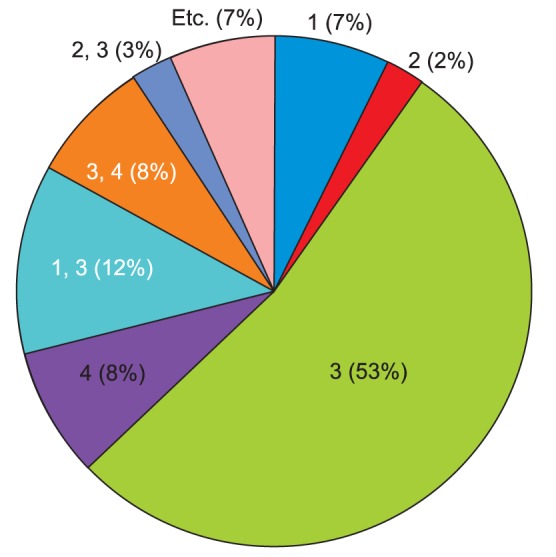
The ratio of patients who visited our clinic with a chief complaint of clicking sound (34.5%) or temporomandibular pain (36.6%) at the initial diagnosis (examination) was the highest. In the evaluation of the depression index, 75.8% of the subjects were normal, 12.9% were moderate, and 11.3% were severe. With regard to non-specific physical symptoms (including pain), 66.5% of the subjects were normal, 17.0% were moderate, and 16.5% were severe. Concerning non-specific physical symptoms (excluding pain), 70.6% of the subjects were normal, 14.4% were moderate, and 15.0% were severe. In terms of the graded chronic pain score, high disability (grade III, IV) was found in 9.3% of the subjects.
CONCLUSION
Among teenage TMD patients, a portion have clinical symptoms and experience severe psychological pressure; hence requiring attention and treatment, as well as understanding the psychological pressure and appropriate treatments for dysfunction.
MeSH Terms
Figure
Reference
-
1. Yang HY, Kim ME. Prevalence and treatment pattern of Korean patients with temporomandibular disorders. Korean J Oral Med. 2009; 34:63–79.2. Kim YK, Kim SG, Im JH, Yun PY. Clinical survey of the patients with temporomandibular joint disorders, using Research Diagnostic Criteria (Axis II) for TMD: preliminary study. J Craniomaxillofac Surg. 2012; 40:366–372. PMID: 21745749.
Article3. Ko MY, Kim MU. Clinical features of the patients with craniomandibular disorders. J Korean Acad Oral Med. 1993; 18:29–41.4. Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992; 6:301–355. PMID: 1298767.5. Yoshimura Y. The terminology of Japanese Society for Temporomandibular Joint. 1st ed. Tokyo: The Japanese Society for Temporomandibular Joint;2001.6. Shiau YY, Chang C. An epidemiological study of temporomandibular disorders in university students of Taiwan. Community Dent Oral Epidemiol. 1992; 20:43–47. PMID: 1547612.
Article7. Chuang SY. Incidence of temporomandibular disorders (TMDs) in senior dental students in Taiwan. J Oral Rehabil. 2002; 29:1206–1211. PMID: 12472858.
Article8. Lee DJ, Kim KS. Epidemiologic study on the patients visited to Dept of Oral Medicine: in the area of Choongnam. J Korean Acad Oral Med. 2006; 31:101–111.9. Okeson JP. American Academy of Orofacial Pain. Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence Pub;1996.10. Hirsch C, Hoffmann J, Türp JC. Are temporomandibular disorder symptoms and diagnoses associated with pubertal development in adolescents? An epidemiological study. J Orofac Orthop. 2012; 73:6–18. PMID: 22234412.
Article11. Magnusson T, Egermark I, Carlsson GE. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J Orofac Pain. 2000; 14:310–319. PMID: 11203765.12. Torii K. Longitudinal course of temporomandibular joint sounds in Japanese children and adolescents. Head Face Med. 2011; 7:17. PMID: 22029896.
Article13. Krogstad BS, Jokstad A, Dahl BL, Vassend O. The reporting of pain, somatic complaints, and anxiety in a group of patients with TMD before and 2 years after treatment: sex differences. J Orofac Pain. 1996; 10:263–269. PMID: 9161231.14. Hatch JP, Rugh JD, Sakai S, Saunders MJ. Is use of exogenous estrogen associated with temporomandibular signs and symptoms? J Am Dent Assoc. 2001; 132:319–326. PMID: 11258088.
Article15. Kang SC, Lee DG, Choi JH, Kim ST, Kim YK, Ahn HJ. Association between estrogen receptor polymorphism and pain susceptibility in female temporomandibular joint osteoarthritis patients. Int J Oral Maxillofac Surg. 2007; 36:391–394. PMID: 17391927.
Article16. List T, Wahlund K, Wenneberg B, Dworkin SF. TMD in children and adolescents: prevalence of pain, gender differences, and perceived treatment need. J Orofac Pain. 1999; 13:9–20. PMID: 10425964.17. Kim BS, Kim YK, Yun PY, Lee E, Bae J. The effects of estrogen receptor α polymorphism on the prevalence of symptomatic temporomandibular disorders. J Oral Maxillofac Surg. 2010; 68:2975–2979. PMID: 20656393.
Article18. Plesh O, Sinisi SE, Crawford PB, Gansky SA. Diagnoses based on the Research Diagnostic Criteria for Temporomandibular Disorders in a biracial population of young women. J Orofac Pain. 2005; 19:65–75. PMID: 15779541.19. Kim C, Shin ES, Chung JW. Impacts of depression, somatization, and jaw disability on graded chronic pain in TMD patients. J Korean Acad Oral Med. 2005; 30:353–360.20. Roh HS, Lim HS, Chung SC. Reliability, validity, sensitivity and specificity of the Korean version of research diagnostic criteria for temporomandibular disorders axis II depression scale. J Korean Acad Oral Med. 2004; 29:421–433.21. Helkimo M. Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state. Sven Tandlak Tidskr. 1974; 67:101–121. PMID: 4524733.22. Ferrari R, Leonard MS. Whiplash and temporomandibular disorders: a critical review. J Am Dent Assoc. 1998; 129:1739–1745. PMID: 9854925.
Article23. Yun PY, Kim YK. The role of facial trauma as a possible etiologic factor in temporomandibular joint disorder. J Oral Maxillofac Surg. 2005; 63:1576–1583. PMID: 16243173.
Article24. Kamisaka M, Yatani H, Kuboki T, Matsuka Y, Minakuchi H. Four-year longitudinal course of TMD symptoms in an adult population and the estimation of risk factors in relation to symptoms. J Orofac Pain. 2000; 14:224–232. PMID: 11203757.25. Kim J, Kim SC, Yoo SK, Shin AW. Factors influencing stress levels of adolescents: with a focus on the impact of positive self-concept and self-confidence. Korean J Youth Stud. 2011; 18:103–126.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on simultation of the mandibular movement of the patients with temporomandibular joint disorder
- A study on the size of condyle and the posterior slope of the articular eminence in patients with temporomandibular joint disorders
- The Study for Treatment fo Temporo-mandibular Joint Pain
- Non-invasive different modalities of treatment for temporomandibular disorders: review of literature
- Evaluation of mandibular condylar bony changes in temporomandibular disorders using Polytome-U images