Pediatr Gastroenterol Hepatol Nutr.
2016 Jun;19(2):139-142. 10.5223/pghn.2016.19.2.139.
The Challenges of Diagnosing and Following Wilson Disease in the Presence of Proteinuria
- Affiliations
-
- 1Department of Pediatrics, Phoenix Children's Hospital, Phoenix, AZ, USA.
- 2Department of Gastroenterology, Yale University Medical Center, New Haven, CT, USA.
- 3Department of Pediatrics, Roseman University of Health Sciences, Las Vegas, NV, USA.
- 4Department of Pediatrics, Texas Children's Hospital, Houston, TX, USA. tamir.miloh@bcm.edu
- KMID: 2328175
- DOI: http://doi.org/10.5223/pghn.2016.19.2.139
Abstract
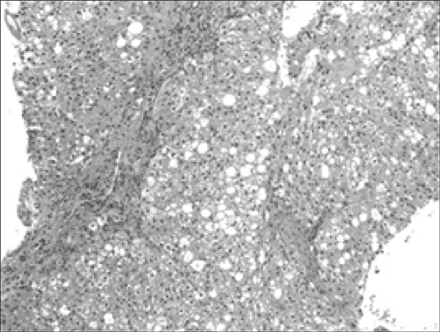
- The coexistence of Wilson disease with Alport syndrome has not previously been reported. The diagnosis of Wilson disease and its ongoing monitoring is challenging when associated with an underlying renal disease such as Alport syndrome. Proteinuria can lead to low ceruloplasmin since it is among serum proteins inappropriately filtered by the damaged glomerulus, and can also lead to increased urinary loss of heavy metals such as zinc and copper. Elevated transaminases may be attributed to dyslipidemia or drug induced hepatotoxicity. The accurate diagnosis of Wilson disease is essential for targeted therapy and improved prognosis. We describe a patient with a diagnosis of Alport syndrome who has had chronic elevation of transaminases eventually diagnosed with Wilson disease based on liver histology and genetics.
Keyword
MeSH Terms
Figure
Reference
-
1. Savige J, Gregory M, Gross O, Kashtan C, Ding J, Flinter F. Expert guidelines for the management of Alport syndrome and thin basement membrane nephropathy. J Am Soc Nephrol. 2013; 24:364–375.
Article2. Roberts EA, Schilsky ML. American Association for Study of Liver Diseases (AASLD). Diagnosis and treatment of Wilson disease: an update. Hepatology. 2008; 47:2089–2111.
Article3. European Association for Study of Liver. EASL clinical practice guidelines: Wilson's disease. J Hepatol. 2012; 56:671–685.4. Morgan SM, Zantek ND. Therapeutic plasma exchange for fulminant hepatic failure secondary to Wilson's disease. J Clin Apher. 2012; 27:282–286.
Article5. Asfaha S, Almansori M, Qarni U, Gutfreund KS. Plasmapheresis for hemolytic crisis and impending acute liver failure in Wilson disease. J Clin Apher. 2007; 22:295–298.
Article6. da Silva GH, Alves AV, Duques P, Sevá-Pereira T, Soares EC, Escanhoela CA. Acute hepatotoxicity caused by enalapril: a case report. J Gastrointestin Liver Dis. 2010; 19:187–190.7. Droste HT, de Vries RA. Chronic hepatitis caused by lisinopril. Neth J Med. 1995; 46:95–98.
Article8. Schattner A, Kozak N, Friedman J. Captopril-induced jaundice: report of 2 cases and a review of 13 additional reports in the literature. Am J Med Sci. 2001; 322:236–240.
Article9. Teslariu O, Nechifor M. Divalent cations levels change in nephrotic syndrome. Rev Med Chir Soc Med Nat Iasi. 2012; 116:883–887.10. Stec J, Podracká L, Pavkovceková O, Kollár J. Zinc and copper metabolism in nephrotic syndrome. Nephron. 1990; 56:186–187.
Article11. Bovio G, Piazza V, Ronchi A, Montagna G, Semeraro L, Galli F, et al. Trace element levels in adult patients with proteinuria. Minerva Gastroenterol Dietol. 2007; 53:329–336.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Wilson's Disease Associated with Somatomotor Status Epileticus
- A Case of Wilson's Disease Compilcated by Hepatocellular Carcinoma
- Successful Pregnancy Outcome in a Patient with Untreated Wilson`s Disease : A Case Report
- Two cases of Wilson disease: MRI findings
- Renal Problems in Wilson Disease