J Korean Soc Transplant.
2013 Jun;27(2):67-71.
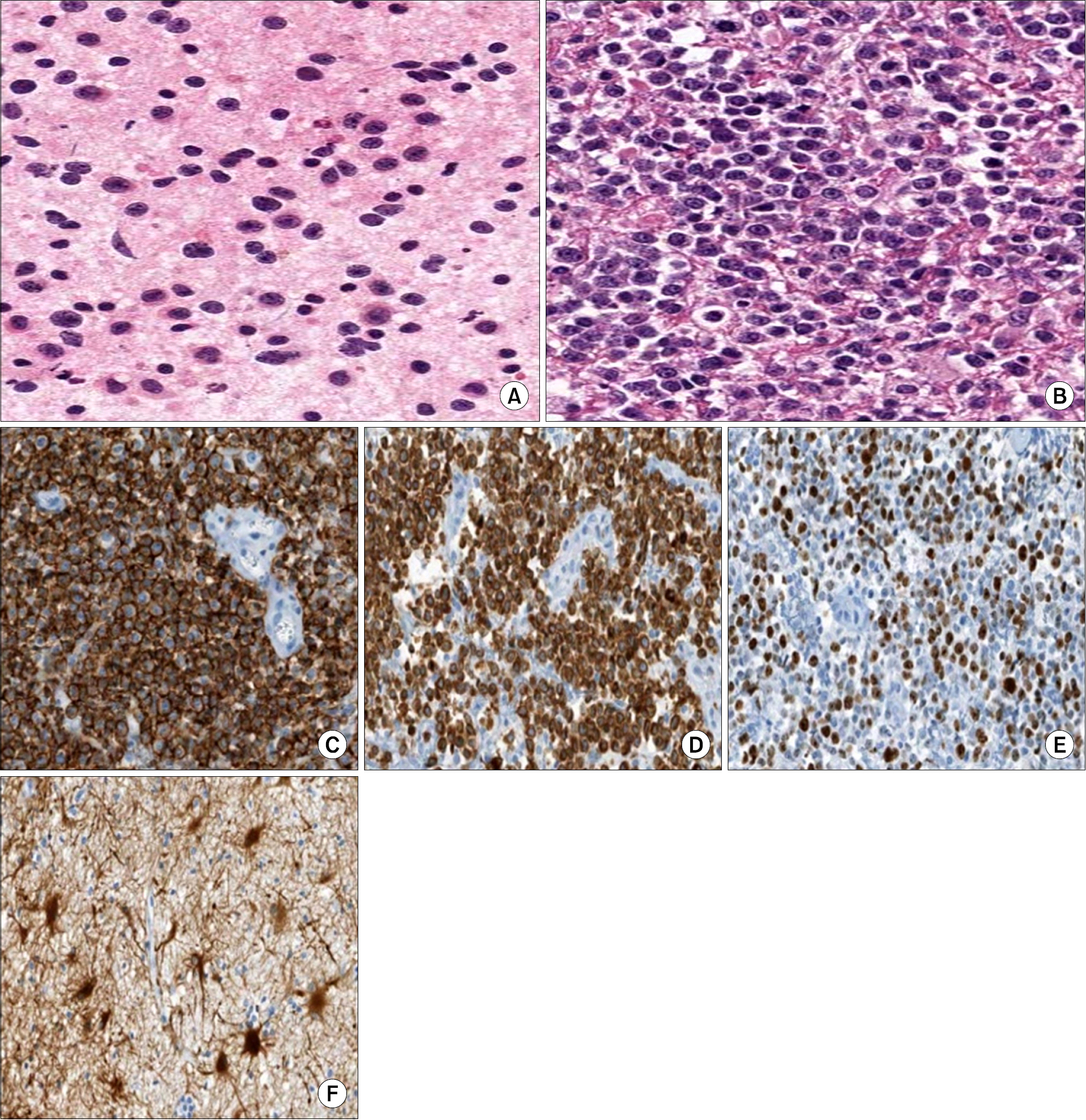
A Brain Tumor from a Posttransplant Lymphoproliferative Disorder in a Kidney Transplant Recipient
- Affiliations
-
- 1Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea. hansy@dsmc.co.kr
- 2Keimyung University Kidney Institute, Daegu, Korea.
Abstract
- Posttransplant lymphoproliferative disorder (PTLD) is a life-threatening complication from organ transplantation. PTLD usually manifests as a mass in the lymph node or an extranodal mass in solid organs, such as the liver, transplanted kidney, tonsil, bone marrow, or spleen. PTLD rarely involves the central nervous system (CNS); however, here we report a case of PTLD that manifested as a brain tumor after kidney transplantation. A 52-year-old man who started peritoneal dialysis due to autosomal dominant polycystic kidney disease, underwent kidney transplantation 4 years ago. After kidney transplantation, he took tacrolimus, mycophenolate mofetil, and steroids. He was admitted to our hospital, complaining of a severe headache. Brain magnetic resonance imaging showed a multifocal, irregular, and round enhancing mass in the left basal ganglia. He underwent a needle biopsy for the enhancing mass and the pathological diagnosis was diffuse large B cell lymphoma. After this mass was confirmed as PTLD by histologic diagnosis, the patient had a reduction in his immunosuppression regimen (including a change from tacrolimus to sirolimus) and was treated with chemotherapy for PTLD. After 20 days, the patient expired from sepsis. PTLD involving the CNS is a rare and serious complication associated with solid organ transplantation. PTLD should be included in the differential diagnosis of brain tumors in recipients of solid organ transplants.
MeSH Terms
-
Basal Ganglia
Biopsy, Needle
Bone Marrow
Brain
Brain Neoplasms
Central Nervous System
Diagnosis, Differential
Headache
Humans
Immunosuppression
Kidney
Kidney Transplantation
Liver
Lymph Nodes
Lymphoma, B-Cell
Lymphoproliferative Disorders
Magnetic Resonance Imaging
Mycophenolic Acid
Organ Transplantation
Palatine Tonsil
Peritoneal Dialysis
Polycystic Kidney, Autosomal Dominant
Sepsis
Spleen
Steroids
Tacrolimus
Transplants
Mycophenolic Acid
Steroids
Tacrolimus
Figure
Reference
-
1). Taylor AL, Marcus R, Bradley JA. Posttransplant lymphoproliferative disorders (PTLD) after solid organ transplantation. Crit Rev Oncol Hematol. 2005; 56:155–67.
Article2). Saadat A, Einollahi B, Ahmadzad-Asl MA, Moradi M, Nafar M, Pourfarziani V, et al. Posttransplantation lymphoproliferative disorders in renal transplant recipients: report of over 20 years of experience. Transplant Proc. 2007; 39:1071–3.
Article3). Martinez AJ. The neuropathology of organ transplantation: comparison and contrast in 500 patients. Pathol Res Pract. 1998; 194:473–86.4). Gerstner ER, Batchelor TT. Primary central nervous system lymphoma. Arch Neurol. 2010; 67:291–7.
Article5). Jagadeesh D, Woda BA, Draper J, Evens AM. Post transplant lymphoproliferative disorders: risk, classification, and therapeutic recommendations. Curr Treat Options Oncol. 2012; 13:122–36.
Article6). Evens AM, Roy R, Sterrenberg D, Moll MZ, Chadburn A, Gordon LI. Posttransplantation lymphoproliferative disorders: diagnosis, prognosis, and current approaches to therapy. Curr Oncol Rep. 2010; 12:383–94.
Article7). Buell JF, Gross TG, Hanaway MJ, Trofe J, Roy-Chaud-hury P, First MR, et al. Posttransplant lymphoproliferative disorder: significance of central nervous system involvement. Transplant Proc. 2005; 37:954–5.
Article8). Cavaliere R, Petroni G, Lopes MB, Schiff D. International Primary Central Nervous System Lymphoma Collaborative Group. Primary central nervous system posttransplantation lymphoproliferative disorder: an International Primary Central Nervous System Lymphoma Collaborative Group Report. Cancer. 2010; 116:863–70.9). Wimmer CD, Rentsch M, Crispin A, Illner WD, Arbogast H, Graeb C, et al. The janus face of immunosuppression: de novo malignancy after renal transplantation: the experience of the Transplantation Center Munich. Kidney Int. 2007; 71:1271–8.10). Snanoudj R, Durrbach A, Leblond V, Caillard S, Hurault De Ligny B, Noel C, et al. Primary brain lymphomas after kidney transplantation: presentation and outcome. Transplantation. 2003; 76:930–7.
Article11). Einollahi B, Lessan-Pezeshki M, Nourbala MH, Simfor-oosh N, Pourfarziani V, Nemati E, et al. Posttransplant lymphoproliferative disorders in kidney transplant recipients: an Iranian multicenter experience. Iran J Kidney Dis. 2008; 2:227–33.12). Castellano-Sanchez AA, Li S, Qian J, Lagoo A, Weir E, Brat DJ. Primary central nervous system posttransplant lymphoproliferative disorders. Am J Clin Pathol. 2004; 121:246–53.
Article13). Phan TG, O'Neill BP, Kurtin PJ. Posttransplant primary CNS lymphoma. Neuro Oncol. 2000; 2:229–38.
Article14). Lim WH, Russ GR, Coates PT. Review of Epstein-Barr virus and posttransplant lymphoproliferative disorder post-solid organ transplantation. Nephrology (Carlton). 2006; 11:355–66.15). Traum AZ, Rodig NM, Pilichowska ME, Somers MJ. Central nervous system lymphoproliferative disorder in pediatric kidney transplant recipients. Pediatr Transplant. 2006; 10:505–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posttransplant Lymphoproliferative Disorder without Epstein-Barr Virus Presented as Small Bowel Perforation in Renal Transplant Recipient: A Case Report
- A case of posttransplantation lymphoproliferative disease developed in renal transplant recipient and treated with rituximab
- Bilateral Conjunctival Mucosa-Associated Lymphoid Tissue Type Lymphoma in a Kidney Transplant Recipient
- Outbreak of Posttransplant Lymphoproliferative Disorder (PTLD) in a Single Center
- Four Cases of Posttransplant Lymphoproliferative Disease (PTLD) Following Renal Transplantation