World J Mens Health.
2013 Dec;31(3):220-225.
Dichotomous Estimation of Prostate Volume: A Diagnostic Study of the Accuracy of the Digital Rectal Examination
- Affiliations
-
- 1Sydney Adventist Hospital Clinical School, University of Sydney, Sydney, NSW, Australia. hwoo@urologist.net.au
Abstract
- PURPOSE
To assess the diagnostic reliability of a dichotomous digital rectal examination (DRE) tool in assessing prostate volume (PV) compared to gold-standard transrectal ultrasound (TRUS) volume measurement.
MATERIALS AND METHODS
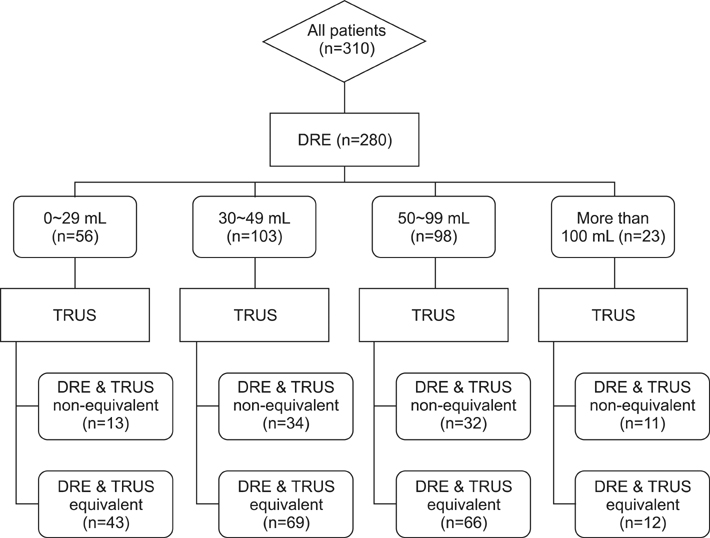
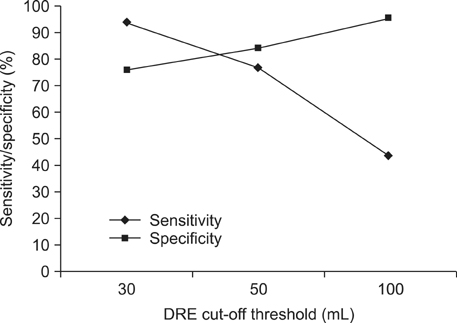
Male patients presenting to a single tertiary referral centre urology practice requiring TRUS were prospectively recruited between January 2010 and August 2011. Size was estimated by DRE immediately prior to TRUS measurement. DRE measurements were classed into four groups: <30 mL , 30 to 49 mL, 50 to 99 mL and >100 mL. The primary outcomes were sensitivity, specificity, and the positive and negative likelihood ratios for a 30 mL cut-off.
RESULTS
Three hundred and three patients were recruited to the study. The median age of the study group was 64.9 years. On TRUS analysis, 244 patients had a PV larger than 30 mL and 139 of them, larger than 50 mL. The median PV was 47 mL with a median International Prostate Symptom Score of 10 and prostatic specific antigen (PSA) of 5.7. When analysed for the ability to identify a gland larger than 30 mL, DRE had a high sensitivity and low negative likelihood ratio. The median PSA level (ng/L) for prostates measured by DRE with a 30 mL cut-off was significantly different with higher median PSA values for volumes larger than 30 mL.
CONCLUSIONS
DRE is a reliable tool for dichotomous assessment of prostatic volumes above 30 mL and 50 mL. These results illustrate the value of re-examining the role of categorical DRE estimations in benign prostatic hyperplasia patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Kumar V, Marr C, Bhuvangiri A, Irwin P. A prospective study of conservatively managed acute urinary retention: prostate size matters. BJU Int. 2000; 86:816–819.
Article2. Jacobsen SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, Guess HA, et al. Natural history of prostatism: risk factors for acute urinary retention. J Urol. 1997; 158:481–487.
Article3. Roehrborn CG, Girman CJ, Rhodes T, Hanson KA, Collins GN, Sech SM, et al. Correlation between prostate size estimated by digital rectal examination and measured by transrectal ultrasound. Urology. 1997; 49:548–557.
Article4. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005; 37:360–363.5. Roehrborn CG. Accurate determination of prostate size via digital rectal examination and transrectal ultrasound. Urology. 1998; 51:19–22.
Article6. Varenhorst E, Berglund K, Löfman O, Pedersen K. Inter-observer variation in assessment of the prostate by digital rectal examination. Br J Urol. 1993; 72:173–176.
Article7. Kijvikai K. Digital rectal examination, serum prostatic specific antigen or transrectal ultrasonography: the best tool to guide the treatment of men with benign prostatic hyperplasia. Curr Opin Urol. 2009; 19:44–48.
Article8. Roehrborn CG, Sech S, Montoya J, Rhodes T, Girman CJ. Interexaminer reliability and validity of a three-dimensional model to assess prostate volume by digital rectal examination. Urology. 2001; 57:1087–1092.
Article9. Ahmad S, Manecksha RP, Cullen IM, Flynn RJ, McDermott TE, Grainger R, et al. Estimation of clinically significant prostate volumes by digital rectal examination: a comparative prospective study. Can J Urol. 2011; 18:6025–6030.10. Bosch JL, Bohnen AM, Groeneveld FP. Validity of digital rectal examination and serum prostate specific antigen in the estimation of prostate volume in community-based men aged 50 to 78 years: the Krimpen Study. Eur Urol. 2004; 46:753–759.
Article11. Collins GN, Lee RJ, McKelvie GB, Rogers AC, Hehir M. Relationship between prostate specific antigen, prostate volume and age in the benign prostate. Br J Urol. 1993; 71:445–450.
Article12. Pinsky PF, Kramer BS, Crawford ED, Grubb RL, Urban DA, Andriole GL, et al. Prostate volume and prostate-specific antigen levels in men enrolled in a large screening trial. Urology. 2006; 68:352–356.
Article13. Yu HJ, Chiang GJ, Chiu TY, Lai MK. Relationship between serum prostate specific antigen concentration and prostate volume. J Formos Med Assoc. 1995; 94:666–670.14. Bohnen AM, Groeneveld FP, Bosch JL. Serum prostate-specific antigen as a predictor of prostate volume in the community: the Krimpen study. Eur Urol. 2007; 51:1645–1652.
Article15. Fowler JE Jr, Bigler SA, Kilambi NK, Land SA. Relationships between prostate-specific antigen and prostate volume in black and white men with benign prostate biopsies. Urology. 1999; 53:1175–1178.
Article16. Chung BH, Hong SJ, Cho JS, Seong DH. Relationship between serum prostate-specific antigen and prostate volume in Korean men with benign prostatic hyperplasia: a multicentre study. BJU Int. 2006; 97:742–746.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The prostate specific antigen in detection of the prostate cancer
- Clinical Significance of Age-Specific Reference Range of PSA
- A Comparative Study for Estimation of Prostatic Volume with Ultrasonography and Computerized Tomography
- Radical Prostatectomy
- Clinical Observation of Decrease of Prostatic Volume in Men with Voiding Symptoms by Means of TRUS