World J Mens Health.
2014 Apr;32(1):61-65.
The Role of Imaging in the Diagnosis of Recurrence of Primary Seminal Vesicle Adenocarcinoma
- Affiliations
-
- 1Nuclear Medicine Unit, Arcispedale Santa Maria Nuova-IRCCS, Reggio Emilia, Italy. martina.sollini@asmn.re.it
- 2Radiology Unit, Arcispedale Santa Maria Nuova-IRCCS, Reggio Emilia, Italy.
- 3Oncology Unit, Arcispedale Santa Maria Nuova-IRCCS, Reggio Emilia, Italy.
- 4Regional Center of Nuclear Medicine, University of Pisa, Pisa, Italy.
Abstract
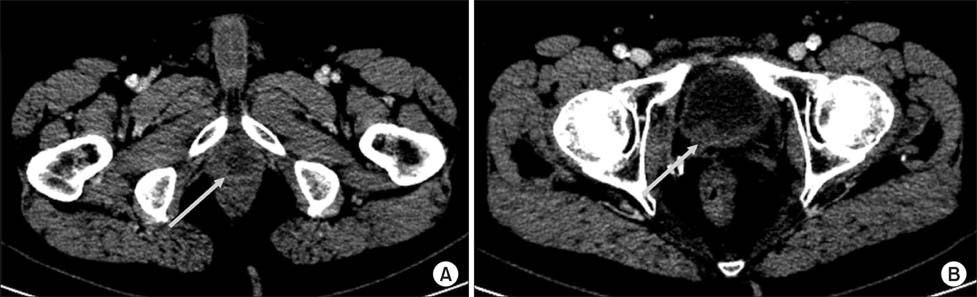
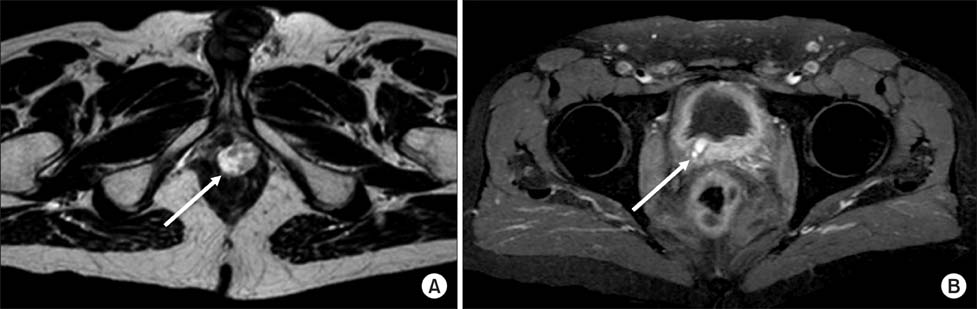
- Primary seminal vesicle (SV) adenocarcinoma is a rare tumor. A small amount of data about the role of imaging to detect tumor recurrence is available. We report the case of a 58-year-old patient with primary SV clear-cell well-differentiated adenocarcinoma. Clinical and instrumental examinations were negative for the 32 months after treatments when computed tomography scan, [18F]fluoro-D-glucose positron emission tomography/computed tomography and pelvic magnetic resonance imaging showed the appearance of a lesion in the left perineal muscle suspected for recurrence. Patient was symptomless. Cytology of the suspected lesion confirmed SV adenocarcinoma recurrence. The combined approach, using radiological and nuclear medicine techniques, seems to be effective in the follow-up of SV adenocarcinoma. Technological advances, together with awareness of this rare tumor, have the potential of improving patients outcomes not only by providing earlier detection and accurate staging, but also by detecting recurrence and thereby avoiding delays and therapeutic dilemmas.
Keyword
MeSH Terms
Figure
Reference
-
1. Egevad L, Ehrnström R, Håkansson U, Grabe M. Primary seminal vesicle carcinoma detected at transurethral resection of prostate. Urology. 2007; 69:778.
Article2. Benson RC Jr, Clark WR, Farrow GM. Carcinoma of the seminal vesicle. J Urol. 1984; 132:483–485.
Article3. Navallas M, Vargas HA, Akin O, Pandit-Taskar N, Fine SW, Eastham JA, et al. Primary seminal vesicle adenocarcinoma. Clin Imaging. 2011; 35:480–482.
Article4. Kreiner B, Denzinger S, Ganzer R, Fritsche HM, Burger M, Wieland WF, et al. Neuroendocrine carcinoma of the seminal vesicles presenting with Lambert Eaton syndrome: a case report. J Med Case Rep. 2010; 4:320.
Article5. Oxley JD, Brett MT, Gillatt DA, Burton P. Seminal vesicle carcinoma. Histopathology. 1999; 34:562–563.
Article6. Tarján M, Ottlecz I, Tot T. Primary adenocarcinoma of the seminal vesicle. Indian J Urol. 2009; 25:143–145.
Article7. Kim B, Kawashima A, Ryu JA, Takahashi N, Hartman RP, King BF Jr. Imaging of the seminal vesicle and vas deferens. Radiographics. 2009; 29:1105–1121.
Article8. Lee BH, Seo JW, Han YH, Kim YH, Cha SJ. Primary mucinous adenocarcinoma of a seminal vesicle cyst associated with ectopic ureter and ipsilateral renal agenesis: a case report. Korean J Radiol. 2007; 8:258–261.
Article9. Zaontz MR, Kass EJ. Ectopic ureter opening into seminal vesicle cyst associated with ipsilateral renal agenesis. Urology. 1987; 29:523–525.
Article10. Versari A. Radionuclide imaging of infection and inflammation: a pictorial case-based atlas. In : Lazzeri E, Signore A, Erba PA, Prandini N, Versari A, D'Errico G, editors. Normal findings from different radiopharmaceuticals and techniques, with variants and pitfalls. 1st ed. New York: Springer Science Business Media, Inc.;2013. p. 1–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Mucinous Adenocarcinoma of a Seminal Vesicle Cyst Associated with Ectopic Ureter and Ipsilateral Renal Agenesis: a Case Report
- Primary Adenocarcinoma of the Seminal Vesicle
- Primary Adenocarcinoma of the Seminal Vesicle: A Case Report
- Cyst of the Seminal Vesicle
- A case of ureteral ectopia draining into seminal vesicle