Tuberc Respir Dis.
2015 Oct;78(4):455-458. 10.4046/trd.2015.78.4.455.
Successful High Flow Nasal Oxygen Therapy for Excessive Dynamic Airway Collapse: A Case Report
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, CHA University, CHA Bundang Medical Center, Seongnam, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. lungdrcho@gmail.com
- KMID: 2320727
- DOI: http://doi.org/10.4046/trd.2015.78.4.455
Abstract
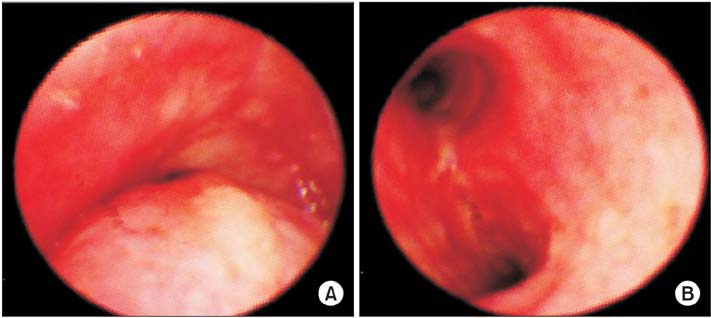
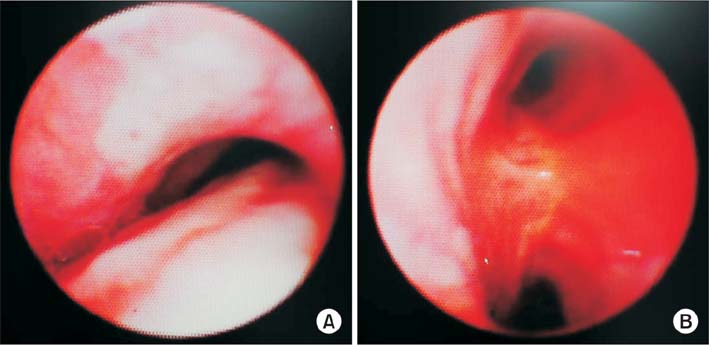
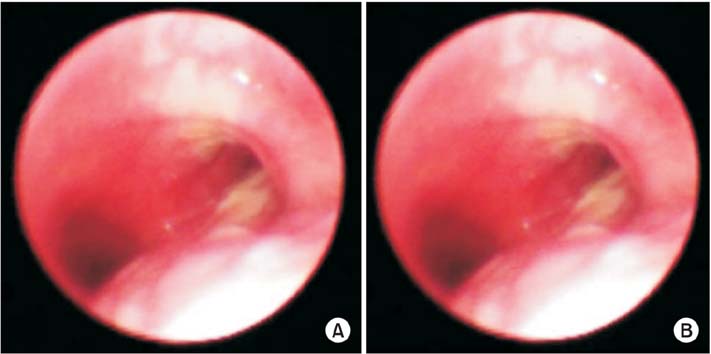
- Excessive dynamic airway collapse (EDAC) is a disease entity of excessive reduction of the central airway diameter during exhalation, without cartilage collapse. An 80-year-old female presented with generalized edema and dyspnea at our hospital. The patient was in a state of acute decompensated heart failure due to pneumonia with respiratory failure. We accordingly managed the patient with renal replacement therapy, mechanical ventilation and antibiotics. Bronchoscopy confirmed the diagnosis of EDAC. We scheduled extubation after the improvement of pneumonia and heart condition. However, extubation failure occurred due to hypercapnic respiratory failure with poor expectoration. Her EDAC was improved in response to high flow nasal oxygen therapy (HFNOT). Subsequently, the patient was stabilized and transferred to the general ward. HFNOT, which generates physiologic positive end expiratory pressure (PEEP) effects, could be an alternative and effective management of EDAC. Further research and clinical trials are needed to demonstrate the therapeutic effect of HFNOT on EDAC.
MeSH Terms
-
Aged, 80 and over
Airway Obstruction
Anti-Bacterial Agents
Bronchoscopy
Cartilage
Diagnosis
Dyspnea
Edema
Exhalation
Female
Heart
Heart Failure
Humans
Oxygen Inhalation Therapy
Oxygen*
Patients' Rooms
Pneumonia
Positive-Pressure Respiration
Renal Replacement Therapy
Respiration, Artificial
Respiratory Insufficiency
Anti-Bacterial Agents
Oxygen
Figure
Reference
-
1. Murgu SD, Colt HG. Description of a multidimensional classification system for patients with expiratory central airway collapse. Respirology. 2007; 12:543–550.2. Murgu SD, Colt HG. Tracheobronchomalacia and excessive dynamic airway collapse. Respirology. 2006; 11:388–406.3. Kalra A, Abouzgheib W, Gajera M, Palaniswamy C, Puri N, Dellinger RP. Excessive dynamic airway collapse for the internist: new nomenclature or different entity? Postgrad Med J. 2011; 87:482–486.4. Park JG, Edell ES. Dynamic airway collapse: different from tracheomalacia. Rev Port Pneumol. 2005; 11:600–602.5. Murgu SD, Cherrison LJ, Colt HG. Respiratory failure due to expiratory central airway collapse. Respir Care. 2007; 52:752–754.6. Nuutinen J. Acquired tracheobronchomalacia: a clinical study with bronchological correlations. Ann Clin Res. 1977; 9:350–355.7. Murgu SD, Colt HG. Tracheobronchomalacia and excessive dynamic airway collapse: novel diagnostic tools clarify the issues. Pulm Perspect. 2005; 22:7–10.8. Murgu SD, Colt HG. Treatment of adult tracheobronchomalacia and excessive dynamic airway collapse: an update. Treat Respir Med. 2006; 5:103–115.9. Gotera C, Diaz Lobato S, Pinto T, Winck JC. Clinical evidence on high flow oxygen therapy and active humidification in adults. Rev Port Pneumol. 2013; 19:217–227.10. Ikeda S, Hanawa T, Konishi T, Adachi M, Sawai S, Chiba W, et al. Diagnosis, incidence, clinicopathology and surgical treatment of acquired tracheobronchomalacia. Nihon Kyobu Shikkan Gakkai Zasshi. 1992; 30:1028–1035.11. Firdose R, Elamin E. Pulmonary edema secondary to dynamic tracheal collapse. J Bronchol. 2004; 11:118–121.12. Carden KA, Boiselle PM, Waltz DA, Ernst A. Tracheomalacia and tracheobronchomalacia in children and adults: an indepth review. Chest. 2005; 127:984–1005.13. Martin JG, Shore S, Engel LA. Effect of continuous positive airway pressure on respiratory mechanics and pattern of breathing in induced asthma. Am Rev Respir Dis. 1982; 126:812–817.14. Sztrymf B, Messika J, Bertrand F, Hurel D, Leon R, Dreyfuss D, et al. Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med. 2011; 37:1780–1786.15. Parke RL, Eccleston ML, McGuinness SP. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care. 2011; 56:1151–1155.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High Flow Nasal Cannula Assisted Tracheostomy for Securing Airways in Patients with Acute Respiratory Distress Induced by Glottic Cancer
- Surgical Correction of Dynamic Nasal Valve Collapse
- Successful application of high-flow nasal cannula in a patient with postoperative respiratory disturbance after bilateral sagittal split ramus osteotomy surgery: A case report
- High-flow nasal oxygenation for anesthetic management
- Diagnosis and Treatment of Dynamic External Nasal Valve Collapse: Application of Alar Batten Graft and Alar Flaring Suture