Tuberc Respir Dis.
2015 Oct;78(4):432-435. 10.4046/trd.2015.78.4.432.
Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium simiae: The First Reported Case in South Korea
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wjkoh@skku.edu
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Korean Institute of Tuberculosis, Osong, Korea.
- 4Department of Microbiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2320722
- DOI: http://doi.org/10.4046/trd.2015.78.4.432
Abstract
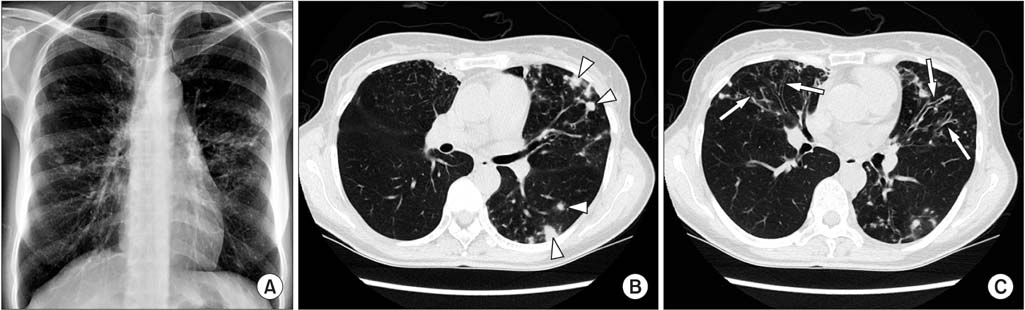
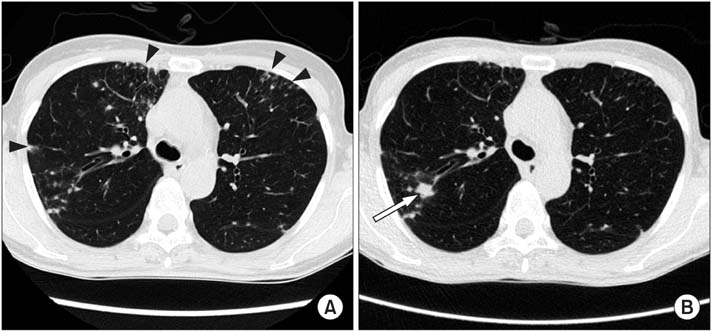
- This is a report of the first South Korean case of a lung disease caused by Mycobacterium simiae. The patient was a previously healthy 52-year-old female. All serial isolates were identified as M. simiae by multi-locus sequencing analysis, based on hsp65, rpoB, 16S-23S rRNA internal transcribed spacer, and 16S rRNA fragments. A chest radiography revealed deterioration, and the follow-up sputum cultures were persistently positive, despite combination antibiotic treatment, including azithromycin, ethambutol, and rifampin. To the best of our knowledge, this is the first confirmed case of a lung disease caused by M. simiae in South Korea.
MeSH Terms
Figure
Reference
-
1. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.2. Maoz C, Shitrit D, Samra Z, Peled N, Kaufman L, Kramer MR, et al. Pulmonary Mycobacterium simiae infection: comparison with pulmonary tuberculosis. Eur J Clin Microbiol Infect Dis. 2008; 27:945–950.3. Velayati AA, Farnia P, Mozafari M, Malekshahian D, Seif S, Rahideh S, et al. Molecular epidemiology of nontuberculous mycobacteria isolates from clinical and environmental sources of a metropolitan city. PLoS One. 2014; 9:e114428.4. van Ingen J, Boeree MJ, Dekhuijzen PN, van Soolingen D. Clinical relevance of Mycobacterium simiae in pulmonary samples. Eur Respir J. 2008; 31:106–109.5. Wang HY, Bang H, Kim S, Koh WJ, Lee H. Identification of Mycobacterium species in direct respiratory specimens using reverse blot hybridisation assay. Int J Tuberc Lung Dis. 2014; 18:1114–1120.6. Ben Salah I, Adekambi T, Raoult D, Drancourt M. rpoB sequence-based identification of Mycobacterium avium complex species. Microbiology. 2008; 154:3715–3723.7. Frothingham R, Wilson KH. Sequence-based differentiation of strains in the Mycobacterium avium complex. J Bacteriol. 1993; 175:2818–2825.8. Turenne CY, Tschetter L, Wolfe J, Kabani A. Necessity of quality-controlled 16S rRNA gene sequence databases: identifying nontuberculous Mycobacterium species. J Clin Microbiol. 2001; 39:3637–3648.9. Adekambi T, Colson P, Drancourt M. rpoB-based identification of nonpigmented and late-pigmenting rapidly growing mycobacteria. J Clin Microbiol. 2003; 41:5699–5708.10. Clinical Laboratory Standards Institute. CLSI document No. M24-A2. Susceptibility testing of mycobacteria, nocardiae, and other aerobic actinomycetes; approved standard. 2nd ed. Wayne: Clinical Laboratory Standards Institute;2011.11. Meier A, Heifets L, Wallace RJ Jr, Zhang Y, Brown BA, Sander P, et al. Molecular mechanisms of clarithromycin resistance in Mycobacterium avium: observation of multiple 23S rDNA mutations in a clonal population. J Infect Dis. 1996; 174:354–360.12. El Sahly HM, Septimus E, Soini H, Septimus J, Wallace RJ, Pan X, et al. Mycobacterium simiae pseudo-outbreak resulting from a contaminated hospital water supply in Houston, Texas. Clin Infect Dis. 2002; 35:802–807.13. Baghaei P, Tabarsi P, Farnia P, Marjani M, Sheikholeslami FM, Chitsaz M, et al. Pulmonary disease caused by Mycobacterium simiae in Iran's national referral center for tuberculosis. J Infect Dev Ctries. 2012; 6:23–28.14. van Ingen J, Totten SE, Heifets LB, Boeree MJ, Daley CL. Drug susceptibility testing and pharmacokinetics question current treatment regimens in Mycobacterium simiae complex disease. Int J Antimicrob Agents. 2012; 39:173–176.15. van Ingen J, van der Laan T, Dekhuijzen R, Boeree M, van Soolingen D. In vitro drug susceptibility of 2275 clinical nontuberculous Mycobacterium isolates of 49 species in The Netherlands. Int J Antimicrob Agents. 2010; 35:169–173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium shinjukuense: The First Reported Case in Korea
- Respiratory Review of 2009: Nontuberculous Mycobacterium
- A Case of Mycobacterium Abscessus Spondylitis
- Lung Disease Caused by Mycobacterium malmoense in an Immunocompetent Patient
- A Case of Mycobacterium abscessus Lung Disease in a Patient with Cystic Fibrosis