Tuberc Respir Dis.
2015 Apr;78(2):112-119. 10.4046/trd.2015.78.2.112.
A Rare Case of Primary Thymic Adenocarcinoma Mimicking Small Cell Lung Cancer
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. yschang@yuhs.ac
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Radiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2320603
- DOI: http://doi.org/10.4046/trd.2015.78.2.112
Abstract
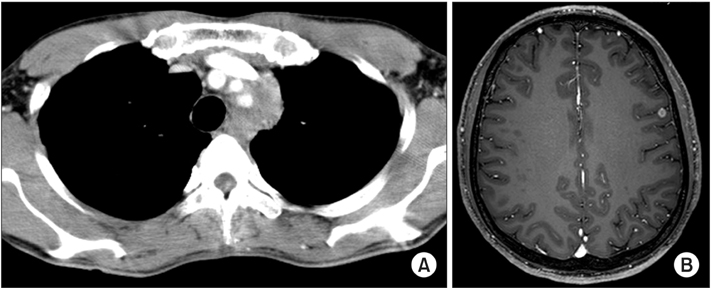
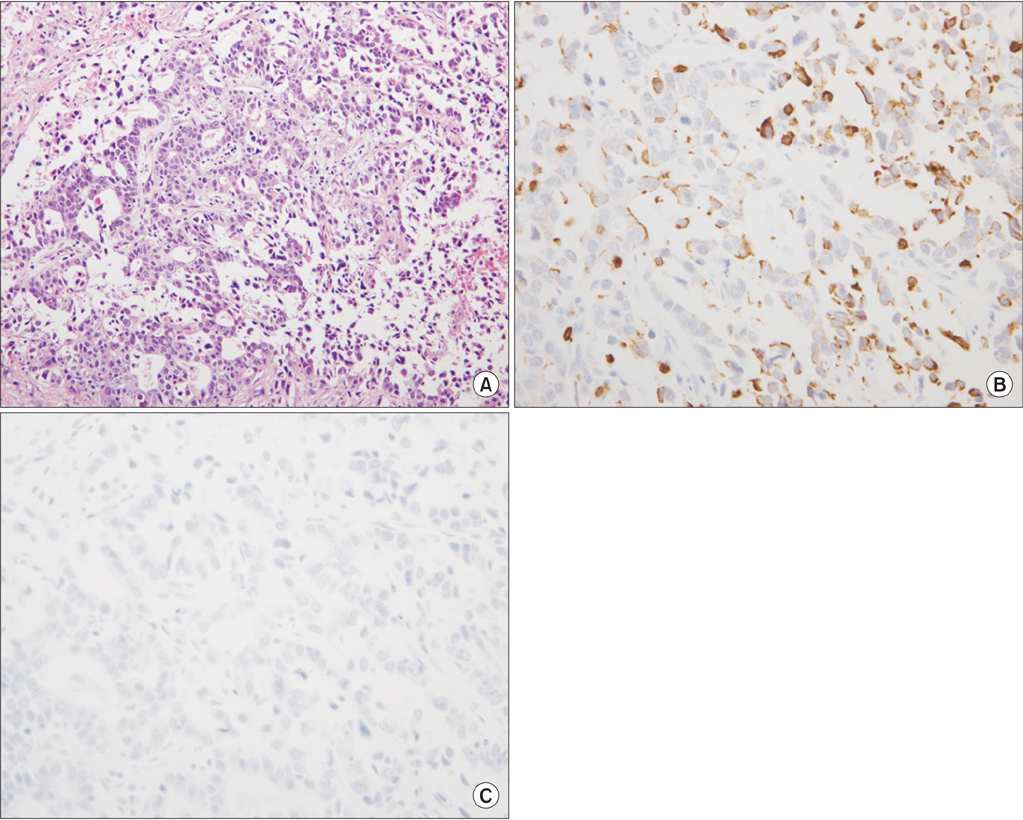
- Primary thymic adenocarcinoma is a very rare malignancy of the anterior mediastinum with no standardized treatment. A 36-year-old male patient presented with hoarseness over the past 3 months. A chest computed tomography (CT) scan showed an infiltrative mass to the proximal vessels and aortic arch in left upper mediastinum (4.1x3.1x5.4 cm). Brain magnetic resonance imaging (MRI) showed focal lesions, suggesting metastasis in the left frontal lobe. A thoracoscopic biopsy of the mediastinal mass confirmed a primary thymic adenocarcinoma forming a glandular structure with atypia of tumor cells. The patient received four cycles of systemic chemotherapy, consisting of etoposide and cisplatin, with concurrent radiotherapy (6,000 cGy/30 fractions) to the mediastinal lesion and the metastatic brain lesion (4,200 cGy/12 fractions). A follow-up chest CT scan and brain MRI showed a decrease in the size of the left upper mediastinal mass and brain lesion. We report a rare case of the primary thymic adenocarcinoma with a literature review.
MeSH Terms
Figure
Cited by 1 articles
-
Cytologic Characteristics of Thymic Adenocarcinoma with Enteric Differentiation: A Study of Four Fine-Needle Aspiration Specimens
Ah-Young Kwon, Joungho Han, Hae-yon Cho, Seokhwi Kim, Heejin Bang, Jiyeon Hyeon
J Pathol Transl Med. 2017;51(5):509-512. doi: 10.4132/jptm.2017.03.22.
Reference
-
1. Jung KW, Won YJ, Kong HJ, Oh CM, Lee DH, Lee JS. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011. Cancer Res Treat. 2014; 46:109–123.2. Kitami A, Suzuki T, Kamio Y, Suzuki S. Chemotherapy of thymic carcinoma: analysis of seven cases and review of the literature. Jpn J Clin Oncol. 2001; 31:601–604.3. Syrios J, Diamantis N, Fergadis E, Katsaros L, Logothetis M, Iakovidou I, et al. Advances in thymic carcinoma diagnosis and treatment: a review of literature. Med Oncol. 2014; 31:44.4. Moran CA, Suster S. Thymic carcinoma: current concepts and histologic features. Hematol Oncol Clin North Am. 2008; 22:393–407.5. Maghbool M, Ramzi M, Nagel I, Bejarano P, Siebert R, Saeedzadeh A, et al. Primary adenocarcinoma of the thymus: an immunohistochemical and molecular study with review of the literature. BMC Clin Pathol. 2013; 13:17.6. Petrini I, Zucali PA, Lee HS, Pineda MA, Meltzer PS, Walter-Rodriguez B, et al. Expression and mutational status of c-kit in thymic epithelial tumors. J Thorac Oncol. 2010; 5:1447–1453.7. Marx A, Strobel P, Badve SS, Chalabreysse L, Chan JK, Chen G, et al. ITMIG consensus statement on the use of the WHO histological classification of thymoma and thymic carcinoma: refined definitions, histological criteria, and reporting. J Thorac Oncol. 2014; 9:596–611.8. Choi WW, Lui YH, Lau WH, Crowley P, Khan A, Chan JK. Adenocarcinoma of the thymus: report of two cases, including a previously undescribed mucinous subtype. Am J Surg Pathol. 2003; 27:124–130.9. Abdul-Ghafar J, Yong SJ, Kwon W, Park IH, Jung SH. Primary thymic mucinous adenocarcinoma: a case report. Korean J Pathol. 2012; 46:377–381.10. Teramoto K, Kawaguchi Y, Hori T, Ishida M, Hashimoto M, Kitamura S, et al. Thymic papillo-tubular adenocarcinoma containing a cyst: report of a case. Surg Today. 2012; 42:988–991.11. Seon HJ, Kim KH, Choi YD, Song SY, Yoon HJ, Kim YH, et al. Angina pectoris caused by the extrinsic compression of coronary artery by primary thymic mucinous adenocarcinoma. Int J Cardiol. 2012; 156:e13–e15.12. Ibuki Y, Okami J, Tomita Y, Fujiwara A, Kanou T, Tokunaga T, et al. Primary papillary carcinoma of the thymus with invasion into subcutaneous tissue through the sternum. J Cardiothorac Surg. 2014; 9:77.13. Kim MJ, Shin HC, Shin KC, Ro JY. Best immunohistochemical panel in distinguishing adenocarcinoma from squamous cell carcinoma of lung: tissue microarray assay in resected lung cancer specimens. Ann Diagn Pathol. 2013; 17:85–90.14. Shin DY, Kim DW, Keam B, Kim TM, Lee SH, Kang CH, et al. The presence of extrathoracic metastasis is more prognostic of survival than Masaoka stage (IVa/IVb) in metastatic thymic epithelial tumor: a retrospective cohort study. Lung Cancer. 2014; 85:320–325.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Early Gastric Cancer Associated with Small Cell Lung Cancer
- A Case of Partial Spontaneous Regression of Non-Small Cell Lung Cancer
- Tripe synchronous primary lung cancer: one case report
- Druggable Targets of Squamous Cell Lung Cancer
- A Case of Primary Small Cell Bronchogenic Carcinoma Detected by Bronchoscopy in a Child