Tuberc Respir Dis.
2014 Jul;77(1):28-33.
A Case of Invasive Pulmonary Aspergillosis with Direct Invasion of the Mediastinum and the Left Atrium in an Immunocompetent Patient
- Affiliations
-
- 1Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea. imekkim@cha.ac.kr
- 2Division of Pulmonology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 3Department of Pathology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
Abstract
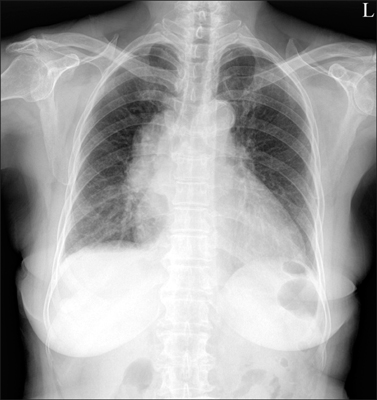
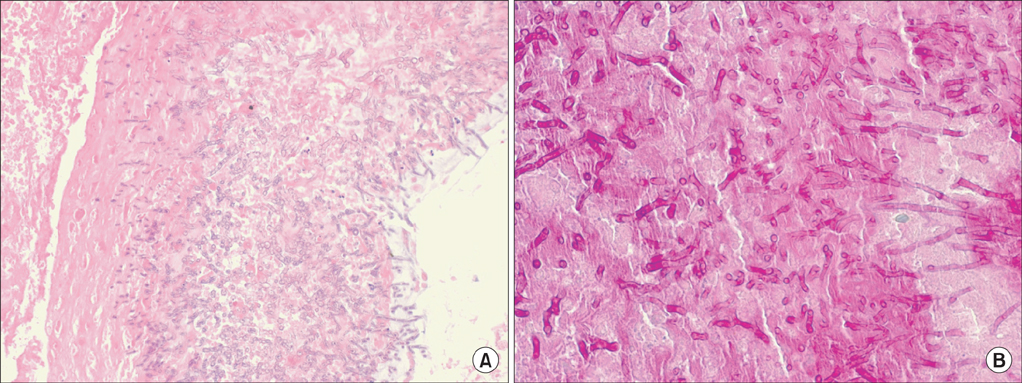
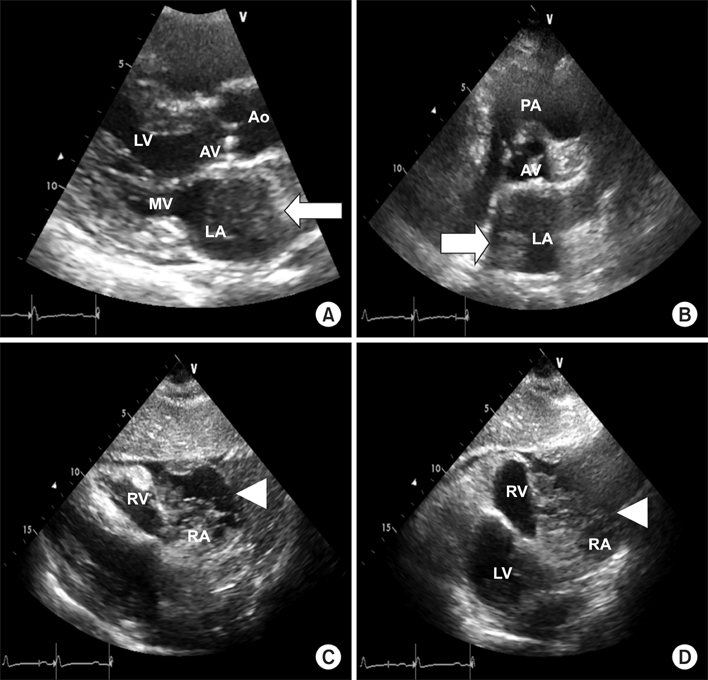
- We report a case of invasive pulmonary aspergillosis invading the mediastinum and the left atrium. A 70-year-old woman was hospitalized for dyspnea. She had been well controlled for her diabetes mellitus and hypertension. The chest X-ray disclosed mediastinal widening, and the computed tomography scan of the chest showed that there was a large mediastinal mass and this lesion extended into the left atrium and right bronchus. The cardiac echocardiography showed that a huge mediastinal cystic mass compressed in the right atrium and a hyperechoic polypoid lesion in the left. The pathology from the bronchoscopic biopsy observed abundant fungal hyphae which was stained with periodic acid-Schiff and Gomori's methenamine silver. Despite the treatment with antifungal agents, she died from cardiac tamponade after three months. Invasive pulmonary aspergillosis, which involves the mediastinum and the heart, is very rare in immunocompetent patients.
MeSH Terms
-
Aged
Antifungal Agents
Biopsy
Bronchi
Cardiac Tamponade
Diabetes Mellitus
Dyspnea
Echocardiography
Female
Heart
Heart Atria*
Heart Neoplasms
Humans
Hypertension
Hyphae
Immunocompetence
Invasive Pulmonary Aspergillosis*
Mediastinal Cyst
Mediastinal Neoplasms
Mediastinum*
Methenamine
Pathology
Thorax
Antifungal Agents
Methenamine
Figure
Reference
-
1. Allam MF, Del Castillo AS, Diaz-Molina C, Navajas RF. Invasive pulmonary aspergillosis: identification of risk factors. Scand J Infect Dis. 2002; 34:819–822.2. Shakoor MT, Ayub S, Ayub Z, Mahmood F. Fulminant invasive aspergillosis of the mediastinum in an immunocompetent host: a case report. J Med Case Rep. 2012; 6:311.3. Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002; 347:408–415.4. Patterson TF, Kirkpatrick WR, White M, Hiemenz JW, Wingard JR, Dupont B, et al. I3 Aspergillus Study Group. Invasive aspergillosis. Disease spectrum, treatment practices, and outcomes. Medicine (Baltimore). 2000; 79:250–260.5. Mennink-Kersten MA, Donnelly JP, Verweij PE. Detection of circulating galactomannan for the diagnosis and management of invasive aspergillosis. Lancet Infect Dis. 2004; 4:349–357.6. Song KH, Lee S, Jang HC, Jeon JH, Park WB, Park KU, et al. Diagnostic usefulness of galactomannan assay for invasive aspergillosis. Infect Chemother. 2009; 41:82–89.7. Aquino VR, Goldani LZ, Pasqualotto AC. Update on the contribution of galactomannan for the diagnosis of invasive aspergillosis. Mycopathologia. 2007; 163:191–202.8. Balloy V, Huerre M, Latge JP, Chignard M. Differences in patterns of infection and inflammation for corticosteroid treatment and chemotherapy in experimental invasive pulmonary aspergillosis. Infect Immun. 2005; 73:494–503.9. Pasqualotto AC, Denning DW. Post-operative aspergillosis. Clin Microbiol Infect. 2006; 12:1060–1076.10. Woods GL, Wood RP, Shaw BW Jr. Aspergillus endocarditis in patients without prior cardiovascular surgery: report of a case in a liver transplant recipient and review. Rev Infect Dis. 1989; 11:263–272.11. Mullen P, Jude C, Borkon M, Porterfield J, Walsh TJ. Aspergillus mural endocarditis. Clinical and echocardiographic diagnosis. Chest. 1986; 90:451–452.12. Hori A, Kami M, Kishi Y, Machida U, Matsumura T, Kashima T. Clinical significance of extra-pulmonary involvement of invasive aspergillosis: a retrospective autopsy-based study of 107 patients. J Hosp Infect. 2002; 50:175–182.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Invasive Pulmonary Aspergillosis Invaded to Thoracic Vertebra in a Immunocompetent Host: A case report
- Concurrent Nocardia Related Brain Abscess and Semi-Invasive Pulmonary Aspergillosis in an Immunocompetent Patient
- Invasive Pulmonary Aspergillosis in a Immunocompetent Patient after Congenital Heart Disease Surgery: A Case Report
- Acute Respiratory Failure from Invasive Pulmonary Aspergillosis in an Immunocompetent Adult: A Case Report
- Invasive Pulmonary Aspergillosis after Influenza A Infection in an Immunocompetent Patient