Tuberc Respir Dis.
2012 Oct;73(4):210-218.
Urine Cotinine for Assessing Tobacco Smoke Exposure in Korean: Analysis of the Korea National Health and Nutrition Examination Survey (KNHANES)
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. NARAE97@yuhs.ac
Abstract
- BACKGROUND
The level of urine cotinine is an indicator of tobacco smoke exposure. The purpose of this study is to investigate urine cotinine for the purpose of assessing the smoking status of Korean smokers and non-smokers exposed to tobacco smoke.
METHODS
The subjects were identified from the 2007-2009 and the 2010 data sets of the Korea National Health and Nutrition Examination Survey (KNHANES). They were assigned as non-smokers, current smokers and ex-smokers. Non-smokers were also divided into three subset groups according to the duration of smoke exposure. Each group was stratified by gender prior to analysis.
RESULTS
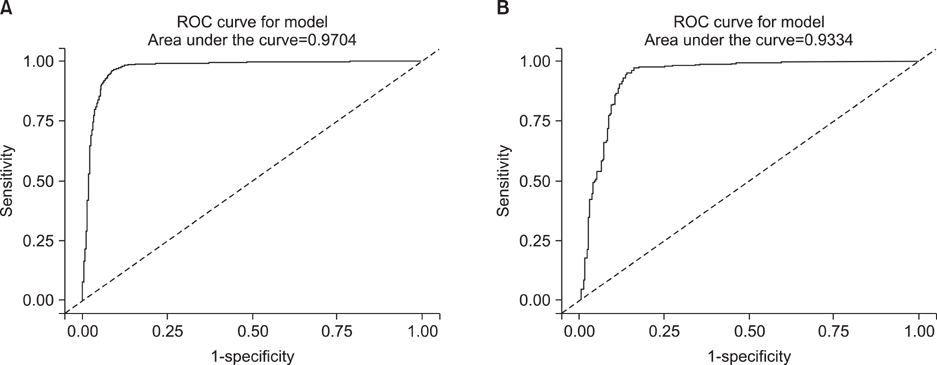
The median value of urine cotinine in the male current smokers was 1,221.93 ng/mL which was the highest among all groups. The difference between levels of urine cotinine for male and the female groups was statistically significant (p<0.01). In the female group, passive smoke exposure groups reported higher urine cotinine levels than non-exposure groups (p=0.01). The cutoff point for the discrimination of current smokers from non-smokers was 95.6 ng/mL in males and 96.8 ng/mL in females. The sensitivity and specificity were 95.2% and 97.1%, respectively, in males, 96.1% and 96.5% in females. However, the determination of urine cotinine level was not useful in distinguishing between passive smoke exposure groups and non-exposure groups.
CONCLUSION
Urine cotinine concentration is a useful biomarker for discriminating non-smokers from current smokers. However, careful interpretation is necessary for assessing passive smoke exposure by urine cotinine concentration.
Keyword
MeSH Terms
Figure
Reference
-
1. Wong SL, Shields M, Leatherdale S, Malaison E, Hammond D. Assessment of validity of self-reported smoking status. Health Rep. 2012. 23:47–53.2. St Helen G, Bernert JT, Hall DB, Sosnoff CS, Xia Y, Balmes JR, et al. Exposure to secondhand smoke outside of a bar and a restaurant and tobacco exposure biomarkers in nonsmokers. Environ Health Perspect. 2012. 120:1010–1016.3. Ino T, Ohtani T, Yoshimi I. Urinary biomarkers for secondhand smoke. J Clin Lab Anal. 2011. 25:354–358.4. Lee K, Lim S, Bartell S, Hong YC. Interpersonal and temporal variability of urinary cotinine in elderly subjects. Int J Hyg Environ Health. 2011. 215:46–50.5. Kang YH, Lee YJ, Kim HK, Yun YH, Jeong SY, Lee JS, et al. Usefulness of urinary cotinine test to distinguish smokers from nonsmokers. Korean J Lab Med. 2003. 23:92–97.6. Wilcox RG, Hughes J, Roland J. Verification of smoking history in patients after infarction using urinary nicotine and cotinine measurements. Br Med J. 1979. 2:1026–1028.7. Jarvis MJ, Tunstall-Pedoe H, Feyerabend C, Vesey C, Saloojee Y. Comparison of tests used to distinguish smokers from nonsmokers. Am J Public Health. 1987. 77:1435–1438.8. Petersen GO, Leite CE, Chatkin JM, Thiesen FV. Cotinine as a biomarker of tobacco exposure: development of a HPLC method and comparison of matrices. J Sep Sci. 2010. 33:516–521.9. Haufroid V, Lison D. Urinary cotinine as a tobacco-smoke exposure index: a minireview. Int Arch Occup Environ Health. 1998. 71:162–168.10. Baheiraei A, Banihosseini SZ, Heshmat R, Mota A, Mohsenifar A. Association of self-reported passive smoking in pregnant women with cotinine level of maternal urine and umbilical cord blood at delivery. Paediatr Perinat Epidemiol. 2012. 26:70–76.11. Benowitz NL, Schultz KE, Haller CA, Wu AH, Dains KM, Jacob P 3rd. Prevalence of smoking assessed biochemically in an urban public hospital: a rationale for routine cotinine screening. Am J Epidemiol. 2009. 170:885–891.12. Goniewicz ML, Eisner MD, Lazcano-Ponce E, Zielinska-Danch W, Koszowski B, Sobczak A, et al. Comparison of urine cotinine and the tobacco-specific nitrosamine metabolite 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) and their ratio to discriminate active from passive smoking. Nicotine Tob Res. 2011. 13:202–208.13. Signorello LB, Cai Q, Tarone RE, McLaughlin JK, Blot WJ. Racial differences in serum cotinine levels of smokers. Dis Markers. 2009. 27:187–192.14. Jee SH, Kim SJ, Won SY, Shin HS, Kim CS, Kim HJ. The study on active and environmental tobacco smoke in biological samples among high school students in Korea. Korean J Epidemiol. 2002. 24:83–92.15. Wall MA, Johnson J, Jacob P, Benowitz NL. Cotinine in the serum, saliva, and urine of nonsmokers, passive smokers, and active smokers. Am J Public Health. 1988. 78:699–701.16. Vine MF, Hulka BS, Margolin BH, Truong YK, Hu PC, Schramm MM, et al. Cotinine concentrations in semen, urine, and blood of smokers and nonsmokers. Am J Public Health. 1993. 83:1335–1338.17. Zielińska-Danch W, Wardas W, Sobczak A, Szołysek-Bołdys I. Estimation of urinary cotinine cut-off points distinguishing non-smokers, passive and active smokers. Biomarkers. 2007. 12:484–496.18. Kwon JT, Nakajima M, Chai S, Yom YK, Kim HK, Yamazaki H, et al. Nicotine metabolism and CYP2A6 allele frequencies in Koreans. Pharmacogenetics. 2001. 11:317–323.19. Nakajima M, Yamamoto T, Kuroiwa Y, Yokoi T. Improved highly sensitive method for determination of nicotine and cotinine in human plasma by high-performance liquid chromatography. J Chromatogr B Biomed Sci Appl. 2000. 742:211–215.20. Lee HR, Kim HK, Yoo JS, Kim KN, Lee SY, Yoo SM, et al. Urine cotinine and environmental tobacco exposure in Korean adolescents. Korean J Fam Med. 2009. 30:31–38.21. Caraballo RS, Giovino GA, Pechacek TF. Self-reported cigarette smoking vs. serum cotinine among U.S. adolescents. Nicotine Tob Res. 2004. 6:19–25.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Estimation of Secondhand Smoke Exposure in Clubs Based on Urinary Cotinine Levels
- Urine Cotinine for Assessing the Association between Secondhand Smoke Exposure and Depression in Adult Non-Smokers in Korea: Analysis of the Korea National Health and Nutrition Examination Survey 2016
- Differences in Environmental Tobacco Smoke Exposure between Self-reporting and Cotinine Test: The Application of Biomarkers
- Relationship between Passive Smoke and Urinary Cotinine Level
- Association between the Urine Cotinine Level and Blood Pressure in Korean Adults with Secondhand Smoke Exposure: Korea National Health and Nutritional Examination Survey 2016–2018