Tuberc Respir Dis.
2012 May;72(5):441-447.
Bronchoscopic Ethanolamine Injection Therapy in Patients with Persistent Air Leak from Chest Tube Drainage
- Affiliations
-
- 1Department of Internal Medicine, Hallym University College of Medicine, Seoul, Korea. kimch2002@hallym.or.kr
- 2Department of Thoracic and Cardiovascular Surgery, Hallym University College of Medicine, Seoul, Korea.
Abstract
- BACKGROUND
Chest tube drainage (CTD) is an indication for the treatment of pneumothorax, hemothroax and is used after a thoracic surgery. But, in the case of incomplete lung expansion, and/or persistent air leak from CTD, medical or surgical thoracoscopy or, if that is unavailable, limited thoracotomy, should be considered. We evaluate the efficacy of bronchoscopic injection of ethanolamine to control the persistent air leak in patients with CTD.
METHODS
Patients who had persistent or prolonged air leak from CTD were included, consecutively. We directly injected 1.0 mL solution of 5% ethanolamine oleate into a subsegmental or its distal bronchus, where it is a probable air leakage site, 1 to 21 times using an injection needle through a fiberoptic bronchoscope.
RESULTS
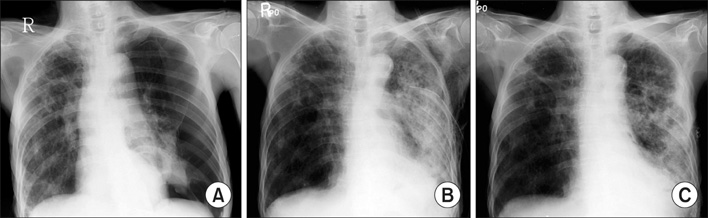
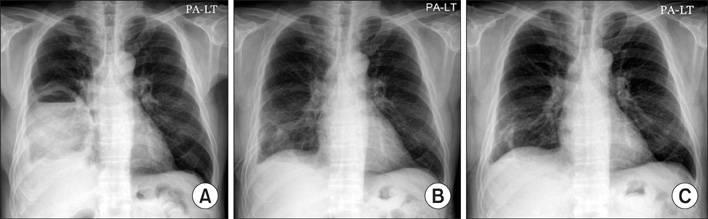
A total of 15 patients were enrolled; 14 cases of spontaneous pneumothorax [idiopathic 9, chronic obstructive pulmonary disease (COPD) 3, post-tuberculosis 2] and one case of empyema associated with broncho-pleural fistula. Of these, five were patients with persistent air leak from CTD, just after a surgical therapy, wedge resection with plication for blebs or bullae. With an ethanolamine injection therapy, 12 were successful but three (idiopathic, COPD and post-tuberculosis) failed, and were followed by a surgery (2 cases) or pleurodesis (1 case). Some adverse reactions, such as fever, chest pain and increased radiographic opacities occurred transiently, but resolved without any further events. With success, the time from the procedure to discharge was about 3 days (median).
CONCLUSION
Bronchoscopic ethanolamine injection therapy may be partially useful in controlling air leakage, and reducing the hospital stay in patients with persistent air leak from CTD.
Keyword
MeSH Terms
Figure
Reference
-
1. Baumann MH, Strange C. The clinician's perspective on pneumothorax management. Chest. 1997. 112:822–828.2. Baumann WR, Ulmer JL, Ambrose PG, Garvey MJ, Jones DT. Closure of a bronchopleural fistula using decalcified human spongiosa and a fibrin sealant. Ann Thorac Surg. 1997. 64:230–233.3. Jessen C, Sharma P. Use of fibrin glue in thoracic surgery. Ann Thorac Surg. 1985. 39:521–524.4. Roksvaag H, Skalleberg L, Nordberg C, Solheim K, Hoivik B. Endoscopic closure of bronchial fistula. Thorax. 1983. 38:696–697.5. Asaki S. Tissue solidification in coping with digestive tract bleeding: hemostatic effect of local injection of 99.5% ethanol. Tohoku J Exp Med. 1981. 134:223–227.6. Fujisawa T, Hongo H, Yamaguchi Y, Shiba M, Kadoyama C, Kawano Y, et al. Intratumoral ethanol injection for malignant tracheobronchial lesions: a new bronchofiberscopic procedure. Endoscopy. 1986. 18:188–191.7. Otani T, Tatsuka T, Kanamaru K, Okuda S. Intramural injection of ethanol under direct vision for the treatment of protuberant lesions of the stomach. Gastroenterology. 1975. 69:123–129.8. Light RW. Management of spontaneous pneumothorax. Am Rev Respir Dis. 1993. 148:245–248.9. Noppen M, Alexander P, Driesen P, Slabbynck H, Verstraeten A. Manual aspiration versus chest tube drainage in first episodes of primary spontaneous pneumothorax: a multicenter, prospective, randomized pilot study. Am J Respir Crit Care Med. 2002. 165:1240–1244.10. van de Brekel JA, Duurkens VA, Vanderschueren RG. Pneumothorax: results of thoracoscopy and pleurodesis with talc poudrage and thoracotomy. Chest. 1993. 103:345–347.11. Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001. 119:590–602.12. Berger R. Pleurodesis for spontaneous pneumothorax. Will the procedure of choice please stand up? Chest. 1994. 106:992–994.13. Colt HG, Russack V, Chiu Y, Konopka RG, Chiles PG, Pedersen CA, et al. A comparison of thoracoscopic talc insufflation, slurry, and mechanical abrasion pleurodesis. Chest. 1997. 111:442–448.14. Light RW, O'Hara VS, Moritz TE, McElhinney AJ, Butz R, Haakenson CM, et al. Intrapleural tetracycline for the prevention of recurrent spontaneous pneumothorax: results of a Department of Veterans Affairs cooperative study. JAMA. 1990. 264:2224–2230.15. Takaoka K, Inoue S, Ohira S. Central bronchopleural fistulas closed by bronchoscopic injection of absolute ethanol. Chest. 2002. 122:374–378.16. Hollaus PH, Lax F, el-Nashef BB, Hauck HH, Lucciarini P, Pridun NS. Natural history of bronchopleural fistula after pneumonectomy: a review of 96 cases. Ann Thorac Surg. 1997. 63:1391–1396.17. Ando M, Yamamoto M, Kitagawa C, Kumazawa A, Sato M, Shima K, et al. Autologous blood-patch pleurodesis for secondary spontaneous pneumothorax with persistent air leak. Respir Med. 1999. 93:432–434.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efects of Autologous Blood Pleurodesis in the Pneumothorax with Persistent Air Leak
- A Case of Severe Air Leak Syndrome Treated with High - Frequency Oscillatory Ventilation ( HFOV )
- Video-Assisted Thoracic Surgery for the Spontaneous Pneumothorax
- Outpatient Chest Tube Management with Using a Panda Pneumothorax Set with a Heimlich Valve
- Bronchial Rupture Following Blunt Chest Trauma: 3 cases reports