Tuberc Respir Dis.
2012 Feb;72(2):173-176.
Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium terrae in a Patient with Bronchiectasis
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Microbiology and Research Institute for Medical Sciences, Infection Signaling Network Research Center, Chungnam National University College of Medicine, Daejeon, Korea. sjshin@cnu.ac.kr
- 3Department of Laboratory Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
Abstract
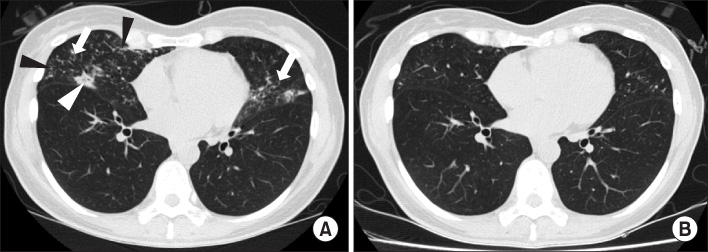
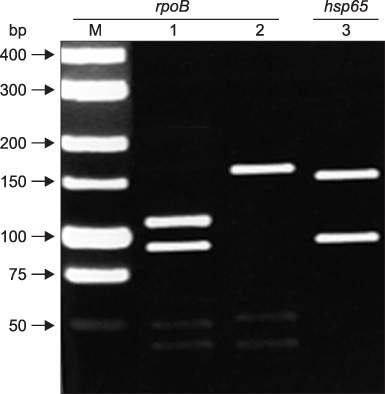
- We report a rare case of lung disease caused by Mycobacterium terrae in a previously healthy woman. A 45-year-old woman was referred to our hospital due to a chronic cough with sputum. A computed tomography scan of the chest revealed bronchiolitis in conjuction with bronchiectasis in both lungs. Nontuberculous mycobacteria were identified and isolated from the bronchoalveolar lavage fluid collected from each lung. All isolates were identified as M. terrae by various molecular methods that characterized the rpoB and hsp65 gene sequences. Antibiotic therapy using clarithromycin, rifampin, and ethambutol improved the patient's condition and successfully resulted in sputum conversion.
MeSH Terms
Figure
Reference
-
1. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.2. Smith DS, Lindholm-Levy P, Huitt GA, Heifets LB, Cook JL. Mycobacterium terrae: case reports, literature review, and in vitro antibiotic susceptibility testing. Clin Infect Dis. 2000. 30:444–453.3. Chen HW, Lai CC, Tan CK. Arthritis caused by Mycobacterium terrae in a patient with rheumatoid arthritis. Int J Infect Dis. 2009. 13:e145–e147.4. Telenti A, Marchesi F, Balz M, Bally F, Böttger EC, Bodmer T. Rapid identification of mycobacteria to the species level by polymerase chain reaction and restriction enzyme analysis. J Clin Microbiol. 1993. 31:175–178.5. Lee H, Park HJ, Cho SN, Bai GH, Kim SJ. Species identification of mycobacteria by PCR-restriction fragment length polymorphism of the rpoB gene. J Clin Microbiol. 2000. 38:2966–2971.6. Alban SM, Sella SR, Miranda RN, Mira MT, Soccol VT. PCR-restriction fragment length polymorphism analysis as a tool for Mycobacterium species identification in lepromas for lepromin production. Lepr Rev. 2009. 80:129–142.7. Clinical and Laboratory Standards Institute (CLSI). Document no, M24-A. Susceptibility testing of mycobacteria, nocardiae, and other aerobic actinomycetes; approved standard. 2003. Wayne, PA: CLSI.8. Wayne LG, Sramek HA. Agents of newly recognized or infrequently encountered mycobacterial diseases. Clin Microbiol Rev. 1992. 5:1–25.9. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006. 129:341–348.10. Kuze F, Mitsuoka A, Chiba W, Shimizu Y, Ito M, Teramatsu T, et al. Chronic pulmonary infection caused by Mycobacterium terrae complex: a resected case. Am Rev Respir Dis. 1983. 128:561–565.11. Krisher KK, Kallay MC, Nolte FS. Primary pulmonary infection caused by Mycobacterium terrae complex. Diagn Microbiol Infect Dis. 1988. 11:171–175.12. Tonner JA, Hammond MD. Pulmonary disease caused by Mycobacterium terrae complex. South Med J. 1989. 82:1279–1282.13. Lee CK, Gi HM, Cho Y, Kim YK, Lee KN, Song KJ, et al. The genomic heterogeneity among Mycobacterium terrae complex displayed by sequencing of 16S rRNA and hsp 65 genes. Microbiol Immunol. 2004. 48:83–90.14. Koh WJ, Lee KS, Kwon OJ, Jeong YJ, Kwak SH, Kim TS. Bilateral bronchiectasis and bronchiolitis at thin-section CT: diagnostic implications in nontuberculous mycobacterial pulmonary infection. Radiology. 2005. 235:282–288.15. Jeon K, Kwon OJ, Lee NY, Kim BJ, Kook YH, Lee SH, et al. Antibiotic treatment of Mycobacterium abscessus lung disease: a retrospective analysis of 65 patients. Am J Respir Crit Care Med. 2009. 180:896–902.16. Koh WJ, Jeon K, Lee NY, Kim BJ, Kook YH, Lee SH, et al. Clinical significance of differentiation of Mycobacterium massiliense from Mycobacterium abscessus. Am J Respir Crit Care Med. 2011. 183:405–410.17. Kim RD, Greenberg DE, Ehrmantraut ME, Guide SV, Ding L, Shea Y, et al. Pulmonary nontuberculous mycobacterial disease: prospective study of a distinct preexisting syndrome. Am J Respir Crit Care Med. 2008. 178:1066–1074.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium shinjukuense: The First Reported Case in Korea
- Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium lentiflavum in a Patient with Bronchiectasis
- The First Korean Case of Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium abscessus Subspecies bolletii in a Patient with Bronchiectasis
- A Case of Hypersensitivity Pneumonitis Caused by Mycobacterium terrae in a Fishery Worker
- Diagnosis and treatment of nontuberculous mycobacterial lung disease