Tuberc Respir Dis.
2011 May;70(5):433-437.
Sarcoidosis Occured after Treatment of Tuberculous Lymphadenitis
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. skysong3@hanmail.net
- 2Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
Abstract
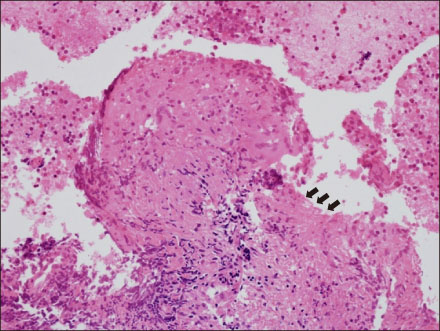
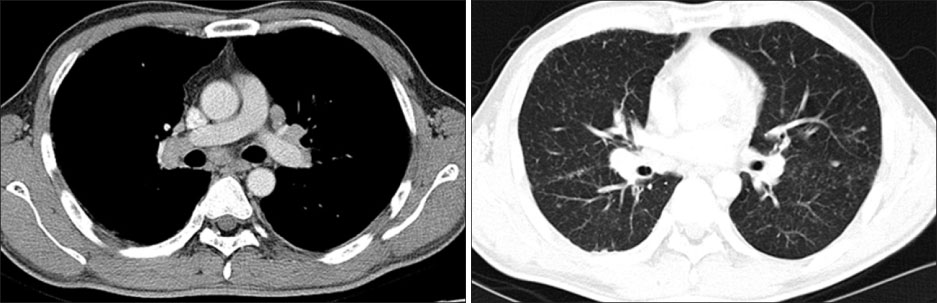
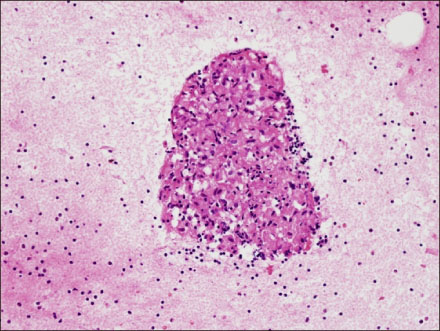
- Sarcoidosis is a multisystemic disorder characterized by the presence of non-caseating granulomas in the involved organ. Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis and is characterized by granuloma with caseous necrosis. The clinical and histological similarity between sarcoidosis and tuberculosis has stimulated research searching for an association between mycobacterium and sarcoidosis. We report a case of a 38-year-old male with sarcoidosis that developed soon after treatment of tuberculous lymphadenitis. He was diagnosed as tuberculous lymphadenitis by microbiological confirmation. He showed clinical improvement after treatment for tuberculosis. One year later, his chest radiography showed bilateral hilar enlargement with diffuse bilateral nodules. A noncaseating granuloma was confirmed by endobronchial ultrasound guided transbronchial needle aspiration and he was diagnosed with sarcoidosis. To our knowledge, this is the first report describing sarcoidosis after treatment of tuberculosis in South Korea.
Keyword
MeSH Terms
Figure
Reference
-
1. House JI, Ayele B, Porco TC, Zhou Z, Hong KC, Gebre T, et al. Assessment of herd protection against trachoma due to repeated mass antibiotic distributions: a cluster-randomised trial. Lancet. 2009. 373:1111–1118.2. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007. 357:2153–2165.3. Semenzato G. ACCESS: a case control etiologic study of sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2005. 22:83–86.4. Drake WP, Newman LS. Mycobacterial antigens may be important in sarcoidosis pathogenesis. Curr Opin Pulm Med. 2006. 12:359–363.5. Gal AA, Koss MN. The pathology of sarcoidosis. Curr Opin Pulm Med. 2002. 8:445–451.6. Scadding JG. Mycobacteria and sarcoidosis. Clinical studies support link. BMJ. 1993. 306:1269–1270.7. Song Z, Marzilli L, Greenlee BM, Chen ES, Silver RF, Askin FB, et al. Mycobacterial catalase-peroxidase is a tissue antigen and target of the adaptive immune response in systemic sarcoidosis. J Exp Med. 2005. 201:755–767.8. Hatzakis K, Siafakas NM, Bouros D. Miliary sarcoidosis following miliary tuberculosis. Respiration. 2000. 67:219–222.9. Mise K, Goic-Barisic I, Puizina-Ivic N, Barisic I, Tonkic M, Peric I. A rare case of pulmonary tuberculosis with simultaneous pulmonary and skin sarcoidosis: a case report. Cases J. 2010. 3:24.10. Carlisle J, Evans W, Hajizadeh R, Nadaf M, Shepherd B, Ott RD, et al. Multiple Mycobacterium antigens induce interferon-gamma production from sarcoidosis peripheral blood mononuclear cells. Clin Exp Immunol. 2007. 150:460–468.11. Chen ES, Wahlström J, Song Z, Willett MH, Wikén M, Yung RC, et al. T cell responses to mycobacterial catalase-peroxidase profile a pathogenic antigen in systemic sarcoidosis. J Immunol. 2008. 181:8784–8796.12. Gupta D, Agarwal R, Aggarwal AN, Jindal SK. Molecular evidence for the role of mycobacteria in sarcoidosis: a meta-analysis. Eur Respir J. 2007. 30:508–516.13. Hajizadeh R, Sato H, Carlisle J, Nadaf MT, Evans W, Shepherd BE, et al. Mycobacterium tuberculosis Antigen 85A induces Th-1 immune responses in systemic sarcoidosis. J Clin Immunol. 2007. 27:445–454.14. Poulter LW, Rossi GA, Bjermer L, Costabel U, Israel-Biet D, Klech H, et al. The value of bronchoalveolar lavage in the diagnosis and prognosis of sarcoidosis. Eur Respir J. 1990. 3:943–944.15. Judson MA. The diagnosis of sarcoidosis. Clin Chest Med. 2008. 29:415–427.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mediastinal & pulmonary sarcoidosis : report of one case and radiologic-pathologic correlation of lymph node enhancement pattern during the treatment
- A Case of Sarcoidosis Associated with Non-tuberculous Mycobacteria
- Axillary Lymph Node Sarcoidosis
- Tuberculous Cervical Lymphadenitis
- Identification of Atypical Mycobacterium with the Polymerase Chain Reaction in Tuberculous Lymphadenitis