Tuberc Respir Dis.
2011 Jan;70(1):43-50.
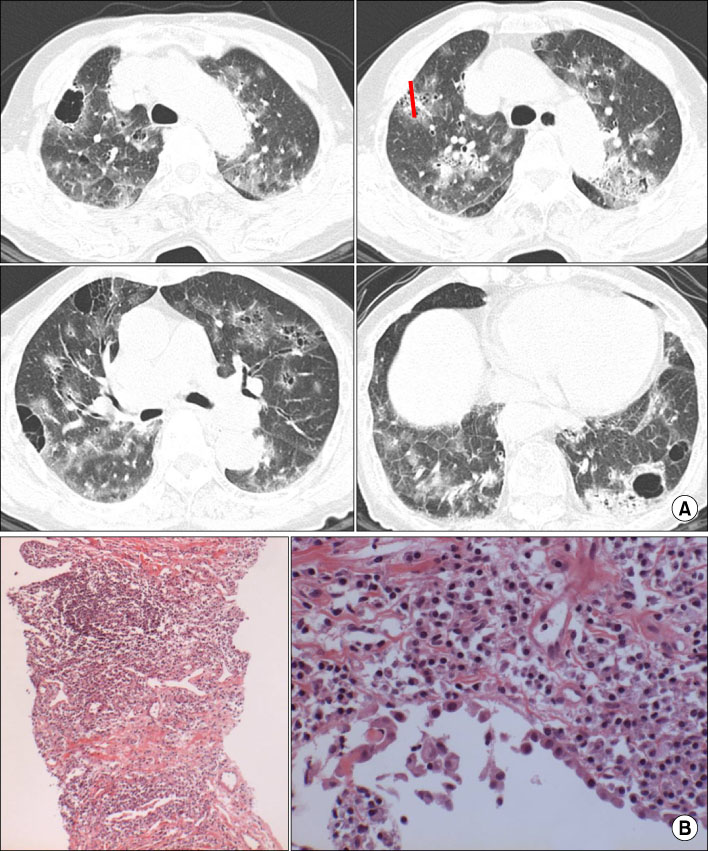
Efficacy of Fluoroscopy-Guided Cutting Needle Lung Biopsy in Patients with Diffuse Infiltrative Lung Disease
- Affiliations
-
- 1Division of Respirology, Department of Medicine, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 2Department of Pathology, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 3Department of Health Promotion Medicine, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea. kjshpc@ewha.ac.kr
Abstract
- BACKGROUND
Open lung biopsy is used for diagnosis of diffuse infiltrative lung diseases (DILD), but it is invasive and relatively expensive procedure. Fluoroscopy-guided cutting needle lung biopsy (FCNLB) has merits of avoidance of admission and rapid diagnosis. But diagnostic accuracy and safety were not well known in the diagnosis of DILD.
METHODS
We included 52 patients (37 men, 15 women) having DILD on HRCT with dyspnea, except the patients who could be confidently diagnosed with clinical and HRCT findings. FCNLB was performed using 16G Ace cut needle (length 1.5 cm, diameter 2 mm) at the area of most active lesion on HRCT. Final diagnoses were made by the consensus.
RESULTS
The mean interval between the HRCT and FCNLB was 4.5 days. Most cases were performed one biopsy during 5~10 minutes. Specific diagnosis was obtained in 43 of 52 biopsies (83%). The most common diagnosis was nonspecific interstitial pneumonia (11 cases) and followed by cryptogenic organizing pneumonia (7 cases), diffuse alveolar hemorrhage and usual interstitial pneumonia (5 cases in each), hypersensitivity pneumonitis (3 cases), tuberculosis and drug induced interstitial pneumonitis (2 cases in each), the others are in one respectively. Mild complication was developed in 9 patients (8 pneumothorax, 1 hemoptysis). Most of complications were regressed without treatment except one case with chest tube insertion for pneumothorax.
CONCLUSION
Fluoroscopy-guided 16 G cutting needle lung biopsy was an useful method for the diagnosis of DILD.
MeSH Terms
Figure
Reference
-
1. Ferguson MK. Thoracoscopy for diagnosis of diffuse lung disease. Ann Thorac Surg. 1993. 56:694–696.2. McElvein RB. The surgical approach to interstitial lung disease. Clin Chest Med. 1982. 3:485–490.3. Arora VK, Gupta R, Johri A. Open lung biopsy in diffuse infiltrative lung disease with progressive dyspnoea: is it useful? Indian J Chest Dis Allied Sci. 2002. 44:203–206.4. Meyer KC. The role of bronchoalveolar lavage in interstitial lung disease. Clin Chest Med. 2004. 25:637–649.5. Herf SM, Suratt PM, Arora NS. Deaths and complications associated with transbronchial lung biopsy. Am Rev Respir Dis. 1977. 115:708–711.6. Wall CP, Gaensler EA, Carrington CB, Hayes JA. Comparison of transbronchial and open biopsies in chronic infiltrative lung diseases. Am Rev Respir Dis. 1981. 123:280–285.7. Lee JH, Lee JC, Kwon JT. Surgical lung biopsy for diffuse infiltrative lung disease. Korean J Thorac Cardiovasc Surg. 2006. 39:844–849.8. Niden AH, Salem F. A safe high-yield technique for cutting needle biopsy of the lung in patients with diffuse lung disease. Chest. 1997. 111:1615–1621.9. Jang I, Kim SW, Yahang JH, Kim JW, Choi JY, Rhie S. Thoracic surgeon's role in differential diagnosis of the interstitial lung disease. Korean J Thorac Cardiovasc Surg. 2006. 39:382–386.10. Klassen KP, Andrews NC. Biopsy of diffuse pulmonary lesions. A seventeen-year experience. Ann Thorac Surg. 1967. 4:117–124.11. Flint A, Martinez FJ, Young ML, Whyte RI, Toews GB, Lynch JP 3rd. Influence of sample number and biopsy site on the histologic diagnosis of diffuse lung disease. Ann Thorac Surg. 1995. 60:1605–1607.12. Manhire A, Charig M, Clelland C, Gleeson F, Miller R, Moss H, et al. Guidelines for radiologically guided lung biopsy. Thorax. 2003. 58:920–936.13. Yankelevitz DF, Vazquez M, Henschke CI. Special techniques in transthoracic needle biopsy of pulmonary nodules. Radiol Clin North Am. 2000. 38:267–279.14. Murphy JM, Gleeson FV, Flower CD. Percutaneous needle biopsy of the lung and its impact on patient management. World J Surg. 2001. 25:373–379.15. Richardson CM, Pointon KS, Manhire AR, Macfarlane JT. Percutaneous lung biopsies: a survey of UK practice based on 5444 biopsies. Br J Radiol. 2002. 75:731–735.16. Glassberg RM, Sussman SK. Life-threatening hemorrhage due to percutaneous transthoracic intervention: importance of the internal mammary artery. AJR Am J Roentgenol. 1990. 154:47–49.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fluoroscopy-Guided Percutaneous Transthoracic Biopsy: Comparison between Fine Needle Aspiration Biopsy and Core Biopsy with an Automated Cutting Needle
- Mixed Herbal Medicine Induced Diffuse Infiltrative Lung Disease: The HRCT and Histopathologic Findings
- Usefulness of CT Fluoroscopy-guided Percutaneous Needle Biopsy in the Presence of Pneumothorax During Biopsy
- Percutaneous Fine Needle Aspiration Biopsy of Lung Masses
- CT-Guided Au tomated Needle Biopsy of Pulmonary Lesions: Analysis of Successful Biopsy Rate and Frequency of Pneumothorax and Hemorrhage using an 18-Gauge Cutting Needle