Tuberc Respir Dis.
2009 Jun;66(6):457-462.
A Case Report of Tuberculous Brain Abscess and Tuberculous Peritonitis Developing Due to Paradoxical Reactions
- Affiliations
-
- 1Department of Internal Medicine, Seoul Red Cross Hospital, Seoul, Korea. sam57993@hanmail.net
Abstract
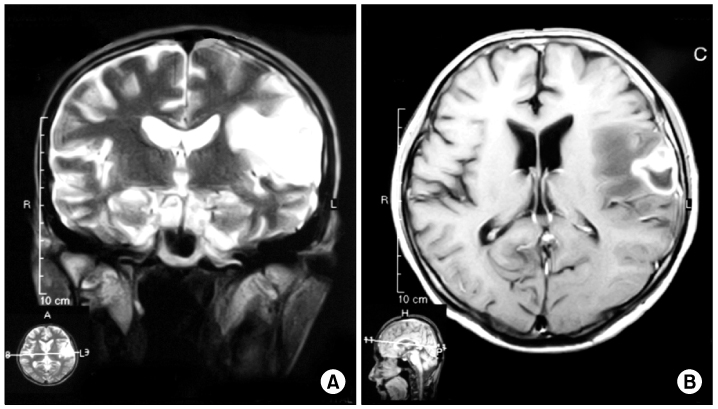
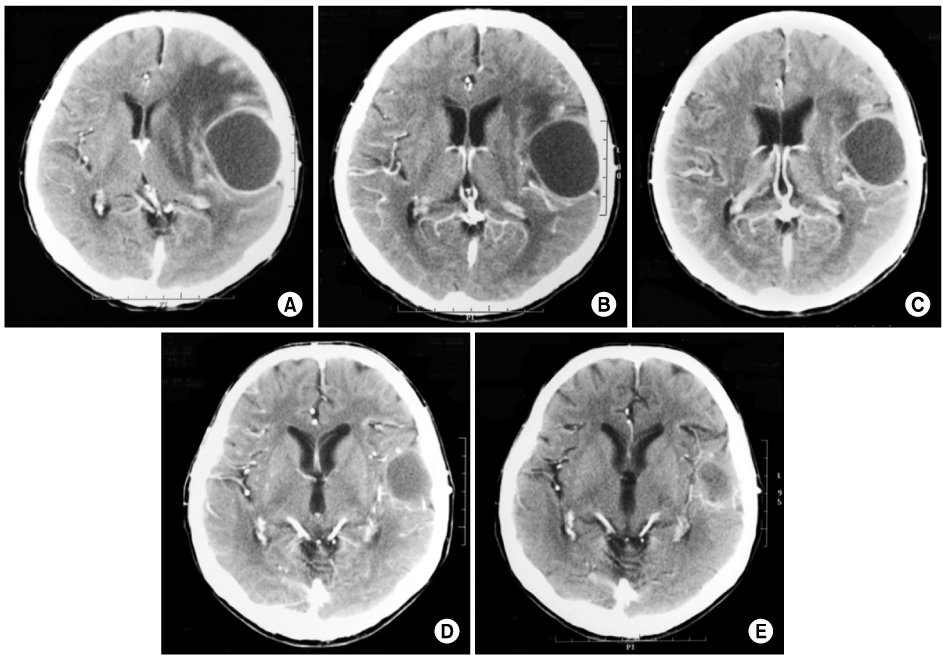
- While receiving appropriate treatment, patients with tuberculosis occasionally have unusual, paradoxical reactions, with transient worsening of lesions or the development of new lesions. This report is a case of tuberculosis brain abscess and tuberculosis peritonitis with intra-abdominal abscess that developed during appropriate anti-tuberculosis chemotherapy. A 45-year-old male patient had been diagnosed as with all-drug susceptible pulmonary tuberculosis with pleurisy. Subsequently, the patient underwent standard treatment with anti-tuberculosis therapy; the pulmonary lesions improved. Three months after initial treatment, the patient developed brain abscesses and peritonitis. With the addition of corticosteroid treatment, the patient's neurologic symptoms were relieved. Exploratory laparotomy with surgical drainage was performed and a diagnosis of tuberculosis peritonitis was confirmed on biopsy. Anti-tuberculosis therapy was continued for 19 months, the patient improved eventually without further complications, although the therapeutic regimen had not been altered. In this case, the paradoxical response to treatment may have been involved in the pathogenesis of disease.
MeSH Terms
Figure
Reference
-
1. Cheng VC, Ho PL, Lee RA, Chan KS, Chan KK, Woo PC, et al. Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur J Clin Microbiol Infect Dis. 2002. 21:803–809.2. Hung SC, Chang SC. New pulmonary lesions during therapy for extrapulmonary tuberculosis. Chest. 1999. 116:1794–1797.3. Onal IK, Bayraktar Y, Unal S. Paradoxical deterioration during the course of antituberculous treatment. J Natl Med Assoc. 2006. 98:954–955.4. Al-Majed SA. Study of paradoxical response to chemotherapy in tuberculous pleural effusion. Respir Med. 1996. 90:211–214.5. Campbell IA, Dyson AJ. Lymph node tuberculosis: a comparison of various methods of treatment. Tubercle. 1977. 58:171–179.6. Kim SH, Chung HY, Lee GD, Shin MG, Jung TS, Jin BC, et al. Clinical characteristics of paradoxical response to chemotherapy in pulmonary tuberculosis. Tuberc Respir Dis. 2002. 53:27–35.7. Narita M, Ashkin D, Hollender ES, Pitchenik AE. Paradoxical worsening of tuberculosis following antiretroviral therapy in patients with AIDS. Am J Respir Crit Care Med. 1998. 158:157–161.8. Ha CY, Kim JY, Kim GC, Ryeom HK, Kim HJ, Lee HJ, et al. An intraperitoneal tuberculous abscess: computed tomography (CT) findings and clinical course. Korean J Med. 2008. 74:243–249.9. Afghani B, Lieberman JM. Paradoxical enlargement or development of intracranial tuberculomas during therapy: case report and review. Clin Infect Dis. 1994. 19:1092–1099.10. Meintjes G, Rangaka MX, Maartens G, Rebe K, Morroni C, Pepper DJ, et al. Novel relationship between tuberculosis immune reconstitution inflammatory syndrome and antitubercular drug resistance. Clin Infect Dis. 2009. 48:667–676.11. Marshall BG, Chambers MA. Central nervous system tuberculosis: the paradox of the host immune response. J Infect. 1998. 36:3–4.12. Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003. 167:603–662.13. Kim JY, Kwon JH, Kim MJ, Chang HW, Hwang JS, Cho KB, et al. Paradoxical response during antituberculous treatment for abdominal tuberculosis. J Korean Radiol Soc. 2006. 55:599–605.14. de Castro CC, de Barros NG, Campos ZM, Cerri GG. CT scans of cranial tuberculosis. Radiol Clin North Am. 1995. 33:753–769.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The CT findings and clinical course of intraperitoneal tuberculous abscess
- A Case of Tuberculous Peritonitis Developed during Chemotherapy for Tuberculous Pleurisy as Paradoxical Response
- A Case of Tuberculous Liver Abscess Developed during Chemotherapy for Tuberculous Peritonitis as Paradoxical Response
- Development of a Tuberculous Liver Abscess as a Paradoxical Response
- Tuberculous Iliopsoas Muscle Abscess Associated with Multiple Intraabdominal and Thoracic Abscesses in 9-year-old Boy