J Korean Ophthalmol Soc.
2016 Jul;57(7):1187-1191. 10.3341/jkos.2016.57.7.1187.
Uremic Optic Neuropathy in Chronic Renal Failure
- Affiliations
-
- 1The Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. samini@yuhs.ac
- 2Hong Samin Optic Nerve Regeneration and Stem Cell Research Institute, Seoul, Korea.
- 3Hong Samin Yonsei Eye Clinic, Seoul, Korea.
- KMID: 2317585
- DOI: http://doi.org/10.3341/jkos.2016.57.7.1187
Abstract
- PURPOSE
To report a case of uremic optic neuropathy occurring in a patient with chronic renal failure.
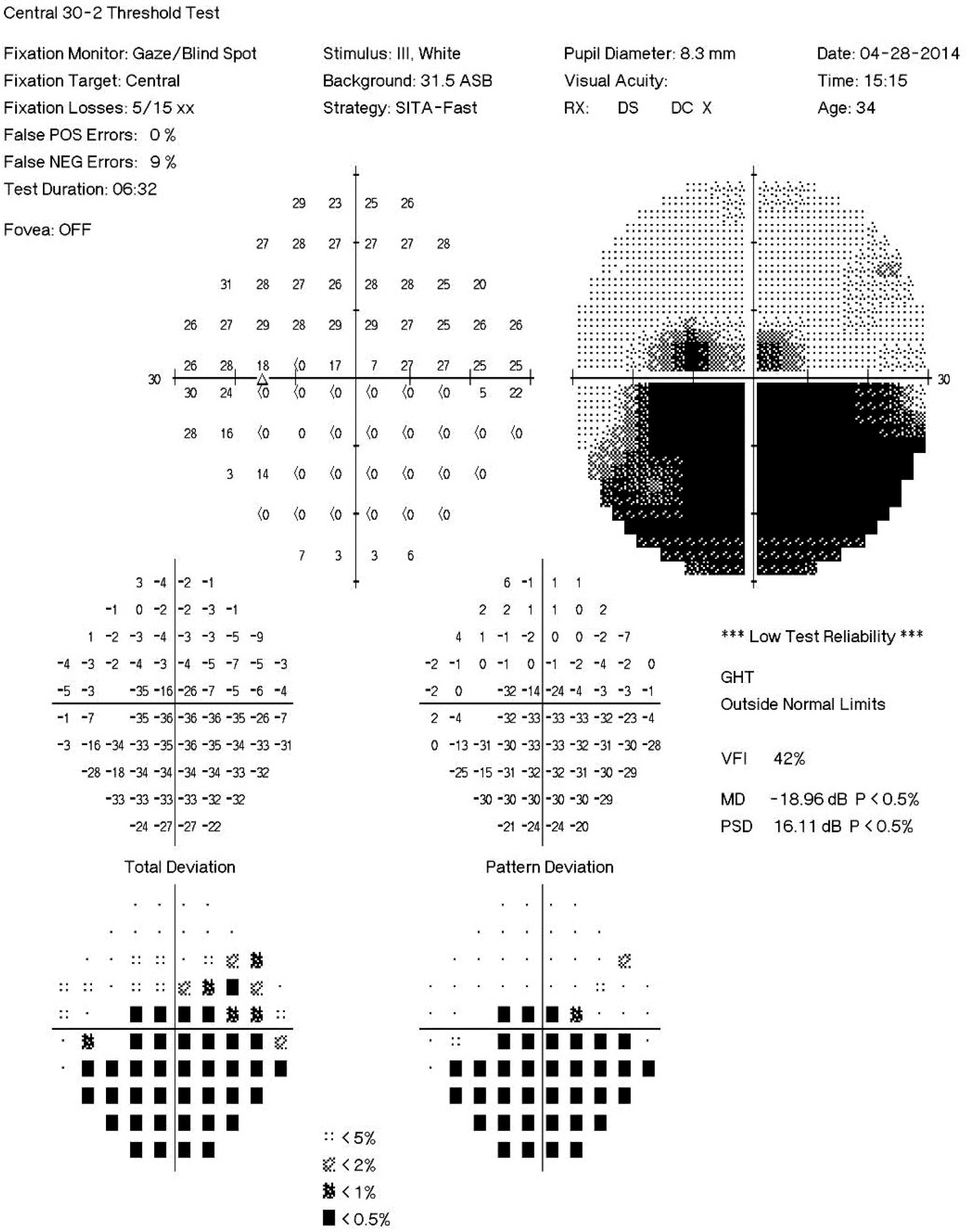
CASE SUMMARY
A 40-year-old male who was diagnosed with chronic renal failure and treated with peritoneal dialysis and hemodialysis for 17 years presented with blurred vision and a moving pain in his left eye for 2 days. The best corrected visual acuity (BCVA) was 0.2 in his left eye, and an inferior altitudinal visual field defect was noted on Humphrey perimetry. Fundus examination and optical coherence tomography showed optic disc swelling in his left eye; the right eye was unremarkable. These findings were compatible with a diagnosis of uremic optic neuropathy or anterior ischemic optic neuropathy of his left eye. After treatment of hemodialysis and intravenous high dose steroid pulse therapy, the BCVA in his left eye was 0.8. However, since he refused oral steroid maintenance therapy, his BCVA later decreased to 0.4. After treatment with subtenon triamcinolone injection, the BCVA in his left eye was 1.0 and showed a stable disease course.
CONCLUSIONS
When patient with chronic renal failure presents with acute decrease in visual acuity and visual field defect, optic neuropathies including uremic optic neuropathy should be considered and prompt hemodialysis and systemic steroid treatment should be done.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Korzets Z, Zeltzer E, Rathaus M, et al. Uremic optic neuropathy. A uremic manifestation mandating dialysis. Am J Nephrol. 1998; 18:240–2.2. Saini JS, Jain IS, Dhar S, Mohan K. Uremic optic neuropathy. J Clin Neuroophthalmol. 1989; 9:131–3. discussion 134–5.3. Winkelmayer WC, Eigner M, Berger O, et al. Optic neuropathy in uremia: an interdisciplinary emergency. Am J Kidney Dis. 2001; 37:E23.
Article4. Nieto J, Zapata MA. Bilateral anterior ischemic optic neuropathy in patients on dialysis: a report of two cases. Indian J Nephrol. 2010; 20:48–50.
Article5. Knox DL, Hanneken AM, Hollows FC, et al. Uremic optic neuropathy. Arch Ophthalmol. 1988; 106:50–4.
Article6. Beri M, Klugman MR, Kohler JA, Hayreh SS. Anterior ischemic optic neuropathy. VII. Incidence of bilaterality and various abdominal factors. Ophthalmology. 1987; 94:1020–8.7. Repka MX, Savino PJ, Schatz NJ, Sergott RC. Clinical profile and long-term implications of anterior ischemic optic neuropathy. Am J Ophthalmol. 1983; 96:478–83.
Article8. Rucker JC, Biousse V, Newman NJ. Ischemic optic neuropathies. Curr Opin Neurol. 2004; 17:27–35.
Article9. Ozdek S, Deren YT, Gurelik G, Hasanreisoglu B. Posterior subtenon triamcinolone, intravitreal triamcinolone and grid laser abdominal for the treatment of macular edema in branch retinal vein occlusion. Ophthalmic Res. 2008; 40:26–31.10. Lin JM, Chiu YT, Hung PT, Tsai YY. Early treatment of severe abdominal macular edema in central retinal vein occlusion with posterior subtenon triamcinolone acetonide. Retina. 2007; 27:180–9.11. Fesharaki H, Kianersi F, Shoyoukhi S. Therapeutic effect of abdominal subtenon methyl prednisolone in anterior ischemic optic abdominal: a randomized clinical trial. Iranian J Ophthalmol. 2011; 23:50–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Posterior Ischemic Optic Neuropathy associated with Hemodialysis in a patient with Chronic Renal Failure
- The Etiology of Optic Neuropathy
- Ocular Manifestations in Patients with Chronic Renal Failure
- Atypical Hemolytic Uremic Syndrome Associated with Streptococcus pneumoniae Infection
- Analysis on the Uremic Bleeding in Patients of Chronic Renal Failure