Korean J Urol.
2013 Feb;54(2):95-99.
Influence of Type of Nocturia and Lower Urinary Tract Symptoms on Therapeutic Outcome in Women Treated With Desmopressin
- Affiliations
-
- 1Department of Urology, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. ksw1227@catholic.ac.kr
Abstract
- PURPOSE
To investigate the type of nocturia and concomitant voiding dysfunction (VD) and the effect of desmopressin treatment on nocturia in women.
MATERIALS AND METHODS
We reviewed 84 women who experienced more than 2 nocturia episodes as recorded on a pretreatment frequency volume chart and who were treated with desmopressin. All patients underwent history taking, physical examination, urinalysis, International Prostate Symptom Score assessment, completion of a urinary sensation scale, and completion of a 3 day frequency volume chart. Nocturia was divided into nocturnal polyuria (NP), reduced nocturnal bladder capacity (RNBC), and mixed type. After treatment with desmopressin, a reduction in nocturia of over 50% compared with baseline was regarded as effective.
RESULTS
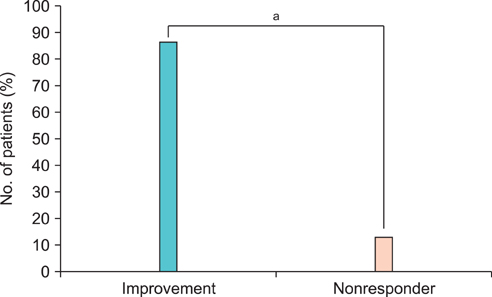
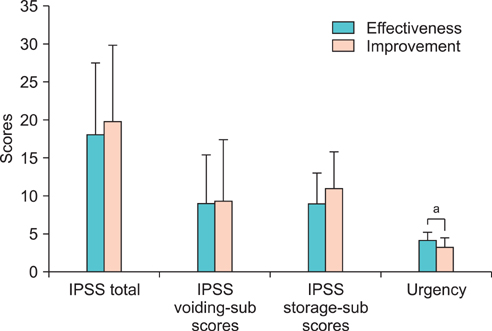
Among 84 women, the most common concomitant VD was overactive bladder (OAB, 60.7%). NP was observed in 70.2% (59/84) of the women, RNBC in 7.1% (6/84), and mixed type in 22.6% (19/84). After medication with desmopressin, 73 women (86.9%) showed a significantly reduced number of nocturia episodes (1.4+/-1.5) compared with baseline (3.7+/-1.3, p<0.05). Eleven women (13.1%) did not show improvement. Of the 73 women who showed improvement, 41 women showed a reduction of more than 50% over baseline, and these women had a lower baseline urgency grade.
CONCLUSIONS
In the majority of women, nocturia coexisted with other VD such as OAB. Treatment with desmopressin effectively reduced the nocturia. However, other lower urinary tract symptoms (LUTS) such as urgency may reduce the effect of desmopressin. Therefore, consideration of concomitant LUTS seems to be necessary to increase the treatment effect of desmopressin on nocturia in women.
MeSH Terms
Figure
Reference
-
1. Middelkoop HA, Smilde-van den, Neven AK, Kamphuisen HA, Springer CP. Subjective sleep characteristics of 1,485 males and females aged 50-93: effects of sex and age, and factors related to self-evaluated quality of sleep. J Gerontol A Biol Sci Med Sci. 1996. 51:M108–M115.2. Yoshimura K, Terada N, Matsui Y, Terai A, Kinukawa N, Arai Y. Prevalence of and risk factors for nocturia: analysis of a health screening program. Int J Urol. 2004. 11:282–287.3. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006. 50:1306–1314.4. Yoo SS, Shim BS, Lee DH, Lee HW, Yoon H. Correlation between nocturia and sleep: a questionnaire based analysis. Korean J Urol. 2010. 51:757–762.5. Tikkinen KA, Tammela TL, Huhtala H, Auvinen A. Is nocturia equally common among men and women? A population based study in Finland. J Urol. 2006. 175:596–600.6. Newman DK, Koochaki PE. Characteristics and impact of interrupted sleep in women with overactive bladder. Urol Nurs. 2011. 31:304–312.7. Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol. 2010. 184:440–446.8. Kim SO, Kim JS, Kim HS, Hwang EC, Oh KJ, Kwon D, et al. Age related change of nocturia in women. Int Neurourol J. 2010. 14:245–249.9. Burgio KL, Johnson TM 2nd, Goode PS, Markland AD, Richter HE, Roth DL, et al. Prevalence and correlates of nocturia in community-dwelling older adults. J Am Geriatr Soc. 2010. 58:861–866.10. van Kerrebroeck P, Rezapour M, Cortesse A, Thuroff J, Riis A, Nørgaard JP. Desmopressin in the treatment of nocturia: a double-blind, placebo-controlled study. Eur Urol. 2007. 52:221–229.11. Mattiasson A, Abrams P, Van Kerrebroeck P, Walter S, Weiss J. Efficacy of desmopressin in the treatment of nocturia: a double-blind placebo-controlled study in men. BJU Int. 2002. 89:855–862.12. Lose G, Lalos O, Freeman RM, van Kerrebroeck P. Nocturia Study Group. Efficacy of desmopressin (Minirin) in the treatment of nocturia: a double-blind placebo-controlled study in women. Am J Obstet Gynecol. 2003. 189:1106–1113.13. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.14. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003. 20:327–336.15. Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001. 87:760–766.16. Irwin DE, Abrams P, Milsom I, Kopp Z, Reilly K. EPIC Study Group. Understanding the elements of overactive bladder: questions raised by the EPIC study. BJU Int. 2008. 101:1381–1387.17. Rackley R, Weiss JP, Rovner ES, Wang JT, Guan Z. 037 Study Group. Nighttime dosing with tolterodine reduces overactive bladder-related nocturnal micturitions in patients with overactive bladder and nocturia. Urology. 2006. 67:731–736.18. Smith AL, Wein AJ. Outcomes of pharmacological management of nocturia with non-antidiuretic agents: does statistically significant equal clinically significant? BJU Int. 2011. 107:1550–1554.19. Chang SC, Lin AT, Chen KK, Chang LS. Multifactorial nature of male nocturia. Urology. 2006. 67:541–544.20. Klingler HC, Heidler H, Madersbacher H, Primus G. Nocturia: an Austrian study on the multifactorial etiology of this symptom. Neurourol Urodyn. 2009. 28:427–431.21. Weiss JP, van Kerrebroeck PE, Klein BM, Norgaard JP. Excessive nocturnal urine production is a major contributing factor to the etiology of nocturia. J Urol. 2011. 186:1358–1363.22. Lose G, Mattiasson A, Walter S, Lalos O, van Kerrebroeck P, Abrams P, et al. Clinical experiences with desmopressin for long-term treatment of nocturia. J Urol. 2004. 172:1021–1025.23. Robinson D, Staskin D, Laterza RM, Koelbl H. Defining female voiding dysfunction: ICI-RS 2011. Neurourol Urodyn. 2012. 31:313–316.