J Korean Neurosurg Soc.
2016 Jul;59(4):368-373. 10.3340/jkns.2016.59.4.368.
Risk Factors for Delayed Hinge Fracture after Plate-Augmented Cervical Open-Door Laminoplasty
- Affiliations
-
- 1Department of Neurosurgery, Korea University Guro Hospital, Seoul, Korea. ykapa76@yahoo.co.kr
- 2Department of Neurosurgery, Korea University Anam Hospital, Seoul, Korea.
- 3Department of Neurosurgery, Korea University Ansan Hospital, Ansan, Korea.
- KMID: 2315972
- DOI: http://doi.org/10.3340/jkns.2016.59.4.368
Abstract
OBJECTIVE
Delayed hinge fracture (HF) that develops after cervical open door laminoplasty can be a source of postoperative complications such as axial pain. However, risk factors related to this complication remain unclear. We performed a retrospective clinical series to determine risk factors for delayed HF following plate-only open-door cervical laminoplasty.
METHODS
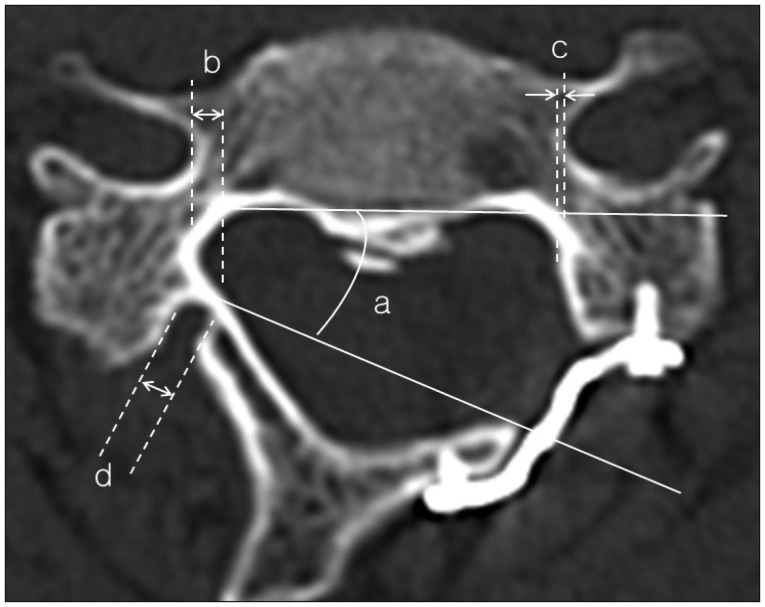
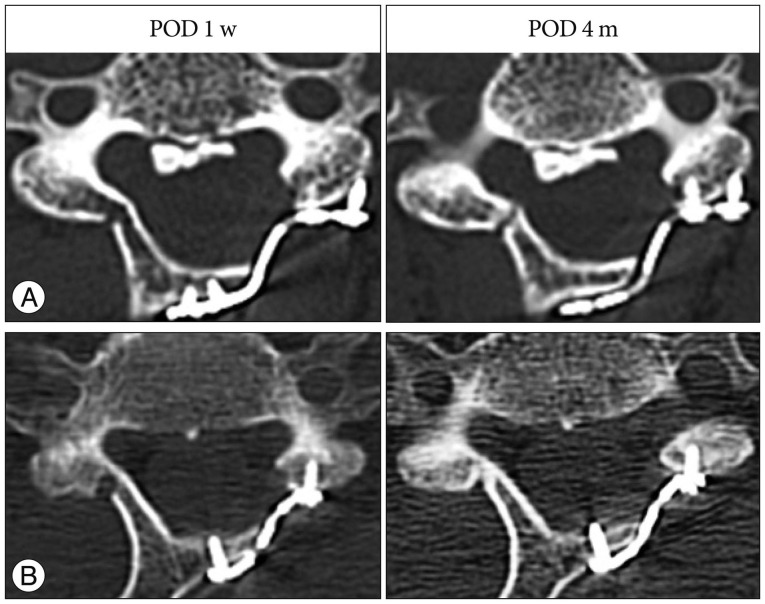
Patients who underwent plate-only open-door laminoplasty and had available postoperative computed tomography (CT) scans (80 patients with 270 laminae) were enrolled. Hinge status, hinge gutter location, open location, hinge width, number of screws used, operation level, and open angle were observed in the CT to determine radiographic outcome. Demographic data were collected as well. Radiographic and clinical parameters were analyzed using univariate and multivariate logistic regression analysis to determine the risk factors for HF.
RESULTS
Univariate logistic regression analysis results indicated poor initial hinge status, medially placed hinge gutter, double screw fixation on the elevated lamina, upper surgical level, and wide open angle as predictors for HF (p<0.05). Initial hinge status seemed to be the most powerful risk factor for HF (p=0.000) and thus was collinear with other variables. Therefore, multivariate logistic regression analysis was performed excluding initial hinge status, and the results indicated that medially placed hinge gutter, double screw fixation on the elevated lamina, and upper surgical level were risk factors for HF after adjustment for other confounding factors.
CONCLUSION
To prevent HF and to draw a successful postoperative outcome after cervical laminoplasty, surgical and clinical precautions should be considered.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Risk Factors for Hinge Fracture Associated with Surgery Following Cervical Open-Door Laminoplasty
Jung Hwan Lee, Chung Kee Chough
Korean J Neurotrauma. 2018;14(2):118-122. doi: 10.13004/kjnt.2018.14.2.118.The Importance of Lamina Size Measurement and Proper Implants Selection before Laminoplasty : Two Case Reports
Dong Hwan Kim, Su Hun Lee, Dong Ha Kim, Kyoung Hyup Nam, In Ho Han, Byung Kwan Choi
Kosin Med J. 2021;36(2):169-174. doi: 10.7180/kmj.2021.36.2.169.
Reference
-
1. Handa Y, Kubota T, Ishii H, Sato K, Tsuchida A, Arai Y. Evaluation of prognostic factors and clinical outcome in elderly patients in whom expansive laminoplasty is performed for cervical myelopathy due to multisegmental spondylotic canal stenosis. A retrospective comparison with younger patients. J Neurosurg. 2002; 96(2 Suppl):173–179. PMID: 12450280.
Article2. Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976). 1988; 13:870–876. PMID: 3143157.
Article3. Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976). 1983; 8:693–699. PMID: 6420895.
Article4. Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976). 1996; 21:1969–1973. PMID: 8883196.5. Kawaguchi Y, Matsui H, Ishihara H, Gejo R, Yoshino O. Axial symptoms after en bloc cervical laminoplasty. J Spinal Disord. 1999; 12:392–395. PMID: 10549702.
Article6. Lee SE, Chung CK, Kim CH, Jahng TA. Symmetrically medial bony gutters for open-door laminoplasty. J Spinal Disord Tech. 2013; 26:E101–E106. PMID: 22935715.
Article7. Lee TT, Manzano GR, Green BA. Modified open-door cervical expansive laminoplasty for spondylotic myelopathy : operative technique, outcome, and predictors for gait improvement. J Neurosurg. 1997; 86:64–68. PMID: 8988083.
Article8. O'Brien MF, Peterson D, Casey AT, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine (Phila Pa 1976). 1996; 21:474–483. discussion 484. PMID: 8658252.9. Ohnari H, Sasai K, Akagi S, Iida H, Takanori S, Kato I. Investigation of axial symptoms after cervical laminoplasty, using questionnaire survey. Spine J. 2006; 6:221–227. PMID: 16651214.
Article10. Park YK, Lee DY, Hur JW, Moon HJ. Delayed hinge fracture after plate-augmented, cervical open-door laminoplasty and its clinical significance. Spine J. 2014; 14:1205–1213. PMID: 24176811.
Article11. Rhee JM, Register B, Hamasaki T, Franklin B. Plate-only open door laminoplasty maintains stable spinal canal expansion with high rates of hinge union and no plate failures. Spine (Phila Pa 1976). 2011; 36:9–14. PMID: 21192219.
Article12. Roselli R, Pompucci A, Formica F, Restuccia D, Di Lazzaro V, Valeriani M, et al. Open-door laminoplasty for cervical stenotic myelopathy : surgical technique and neurophysiological monitoring. J Neurosurg. 2000; 92(1 Suppl):38–43. PMID: 10616056.
Article13. Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H. C5 palsy after decompression surgery for cervical myelopathy : review of the literature. Spine (Phila Pa 1976). 2003; 28:2447–2451. PMID: 14595162.14. Satomi K, Nishu Y, Kohno T, Hirabayashi K. Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976). 1994; 19:507–510. PMID: 8184342.
Article15. Satomi K, Ogawa J, Ishii Y, Hirabayashi K. Short-term complications and long-term results of expansive open-door laminoplasty for cervical stenotic myelopathy. Spine J. 2001; 1:26–30. PMID: 14588365.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hinge Fracture during Cervical Open-door Laminoplasty: Does it Affect Clinical and Radiographic Outcomes?
- Risk Factors for Hinge Fracture Associated with Surgery Following Cervical Open-Door Laminoplasty
- Comparison of Clinical Results according to the Complications after or during Open Door Laminoplasty Surgery for Cervical Myelopathy
- Biomechanical Study of Cervical Posterior Decompression
- Comparison of Midline Splitting versus Unilateral Open Door Laminoplasty and Its Impact on Patient Outcomes