Prog Med Phys.
2014 Dec;25(4):264-270. 10.14316/pmp.2014.25.4.264.
Development and Utility Evaluation of Portable Respiration Training Device for Image-guided Stereotactic Body Radiation Therapy (SBRT)
- Affiliations
-
- 1Korea Institute of Radiological and Medical Sciences, Seoul, Korea.
- 2Department of Medical Physics, Kyonggi University, Suwon, Korea. sikwon@kyonggi.ac.kr
- KMID: 2315766
- DOI: http://doi.org/10.14316/pmp.2014.25.4.264
Abstract
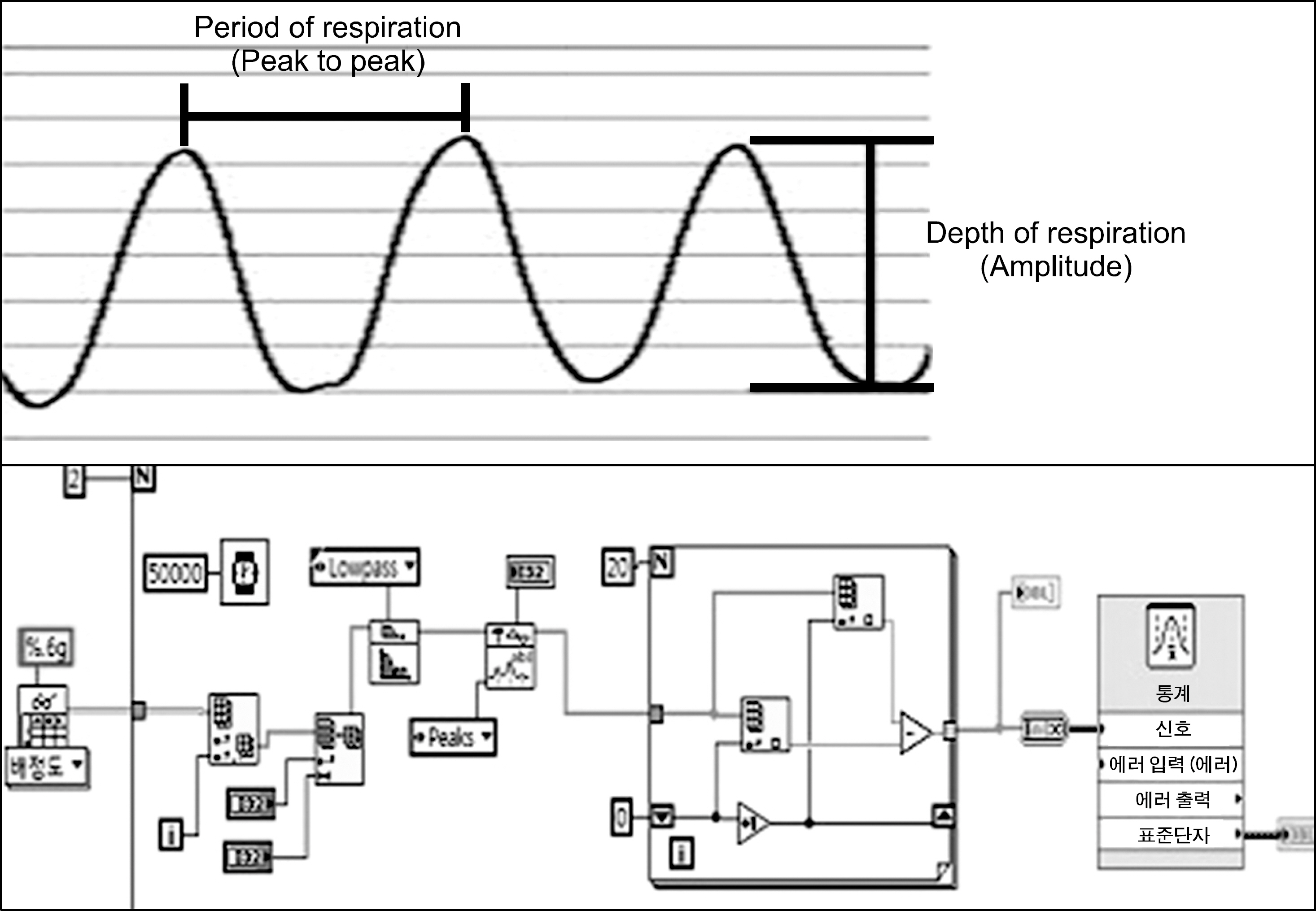
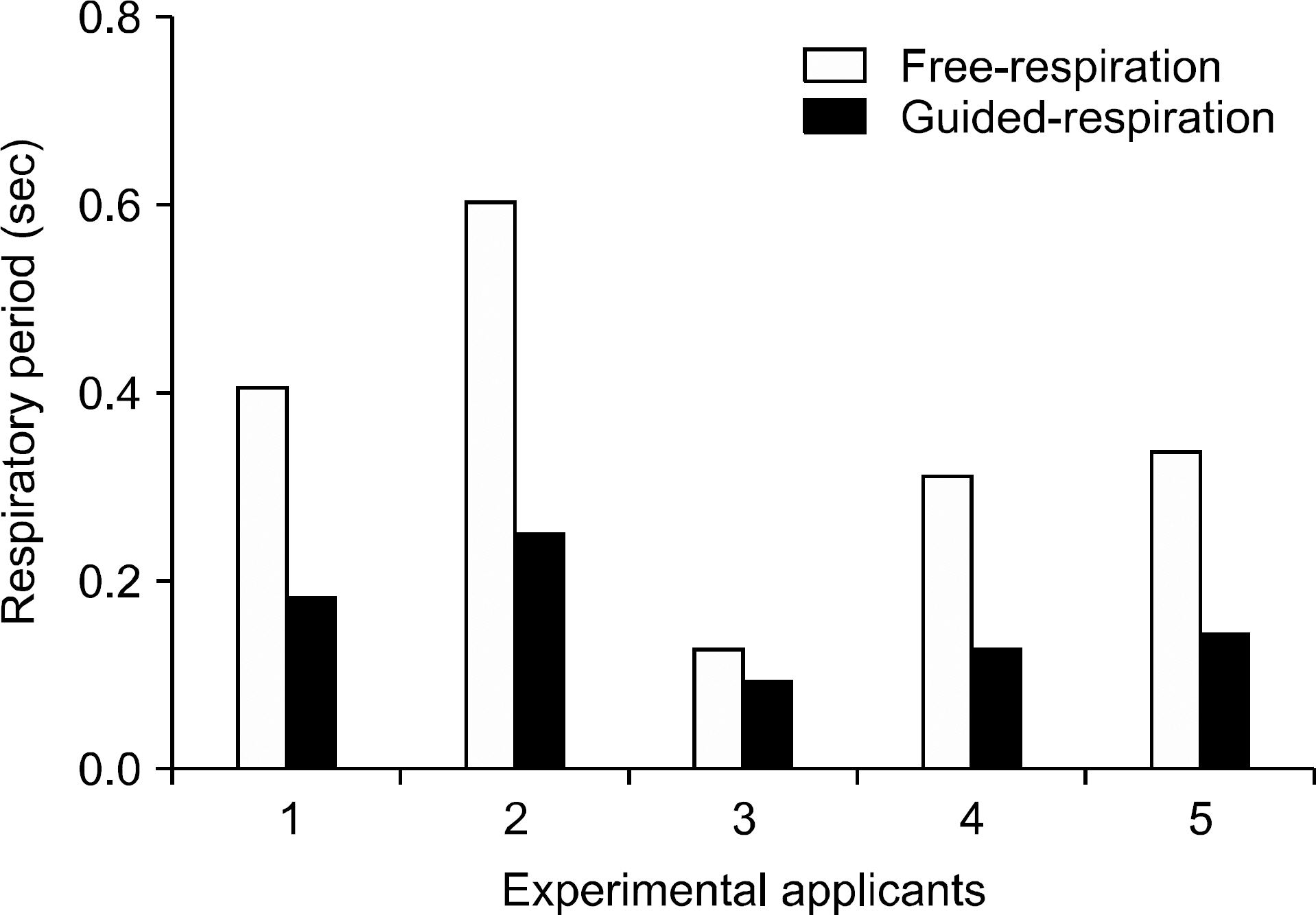
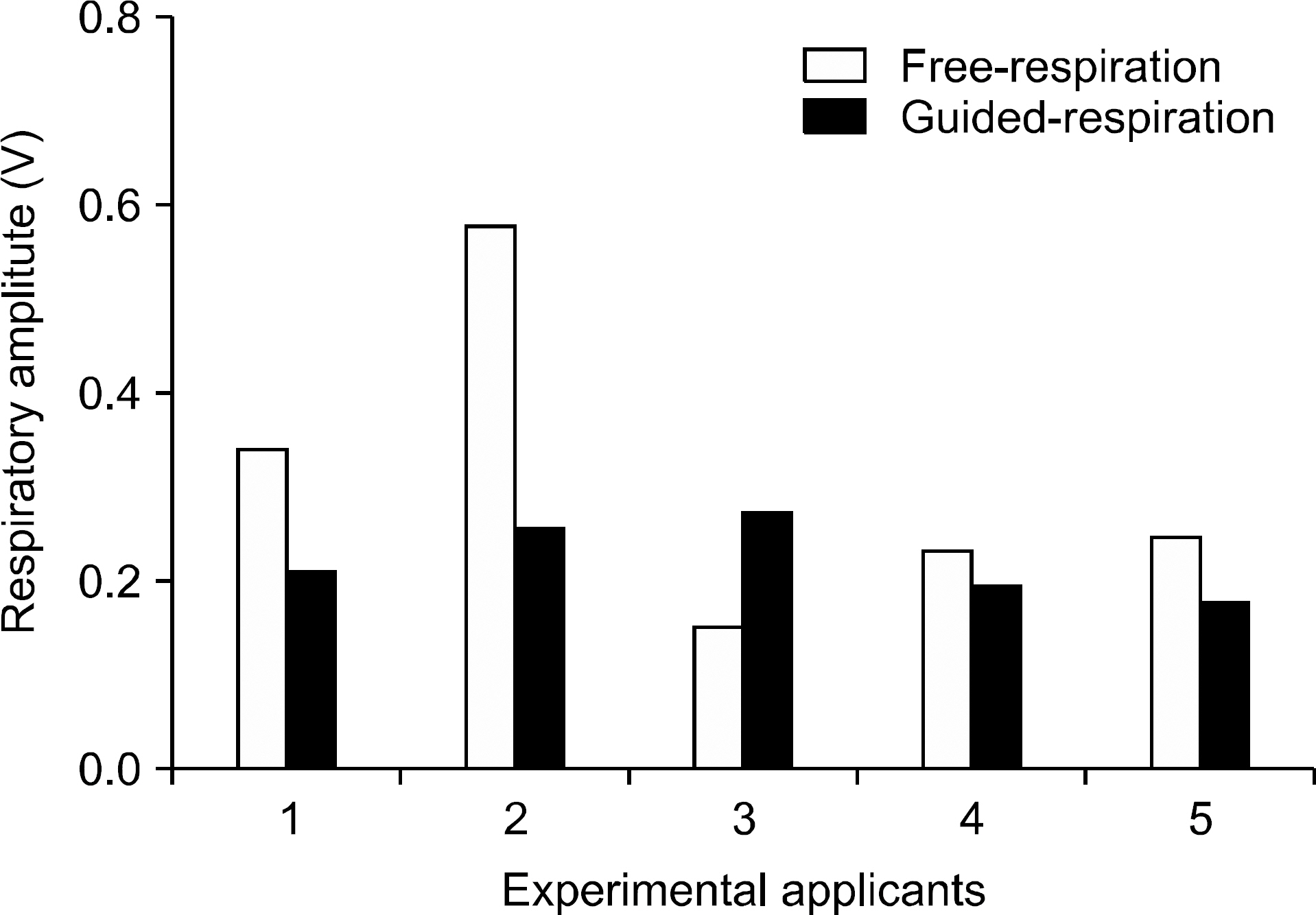
- This study developed a portable respiratory training device to improve breathing stability, which is an important element in using the CyberKnife Synchrony respiratory tracking device, one of the typical Stereotactic Radiation Therapy (SRT) devices. It produced an interface for users to be able to select one of two displays, a graph type and a bar type, supported an auditory system that helps them expect next respiration by improving a sense of rhythm of their respiratory period, and provided comfortable respiratory inducement. By targeting 5 applicants and applying individual respiratory period detected through a self-developed program, it acquired signal data of 'guide respiration' that induces breathing through signal data gained from 'free respiration' and an auditory system, and evaluated the usability by comparing deviation average values of respiratory period and respiratory amplitude. It could be identified that respiratory period decreased 55.74+/-0.14% compared to free respiration, and respiratory amplitude decreased 28.12+/-0.10% compared to free respiration, which confirmed the consistency and stability of respiratory. SBRT, developed based on these results, using the portable respiratory training device, for liver cancer or lung cancer, is evaluated to be able to help reduce delayed treatment time due to respiratory instability and improve treatment accuracy, and if it could be applied to developing respiratory training applications targeting an android-based portable device in the future, even use convenience and economic efficiency are expected.
MeSH Terms
Figure
Reference
-
References
1. Schweikard A, Glosser G, Bodduluri M. Robotic motion compensation for respiratory movement during radiosurgery. Comp Aided Surg. 5:263–277. 2000.
Article2. Schweikard A, Shiomi H, Adler J. Respiration tracking in radiosurgery. Med Phys. 31:2737–2741. 2004.
Article3. Herk V, Rasch C, Lebesque J. V: The probability of correct target dosage: dose population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys. 47(4):1121–135. 2000.4. George R, Kini V, Vedam S, et al. Is the diaphragm motion probability density function normally distributed? Med Phys. 32:396–04. 2005.
Article5. Herk V, Witte M, van der Geer J, et al. Biologic and physical fractionation effects of random geometric errors. Int J Radiat Oncol Biol Phys. 57(5):1460–1471. 2003.6. Yorke E D, Wang L, Rosenzweig K E, et al. Evaluation of deep inspiration breath-hold lung treatment plans with Monte Carlo dose calculation. Int J Radiat Oncol Biol Phys. 53(4):1058–070. 2002.7. American Association of Physicists in Medicine: The Management of Respiratory Motion in Radiation Oncology. Report of AAPM Task Group 76 (. 2006.8. Goitein M, Busse J. Immobilization errors: Some theoretical considerations. Radiology. 117:407–412. 1975.9. Dutreix A. When and how can we improve precision in radiotherapy? Radiother Oncol. 2:275–292. 1984.
Article10. Mah K, VanDyk J, Keane T, et al. Acute radiation-induced pulmonary damage: A clinical study on the response to fractionated radiotherapy. Int J Radiat Oncol Biol Phys. 13:179–188. 1987.11. Langen KM, Jones DTL. Organ motion and its management. Int J Radiat Oncol Biol Phys 265–278 (. 2001.12. Ozhasoglu C, Cheng B, Saw , et al. SYNCHRONY Cyberknife Respiratory Compensation Technology. Med Dosim. 33(2):117–123. 2008.13. Mah D, Hanley J, Rosenweig KE, et al. Technical aspects of the deep inspiration breath-hold technique in the treatment of thoracic cancer. Int J Radiat Oncol Biol Phys. 48:1175–85. 2000.
Article14. Rosenweig KE, Hanley J, Mah D, et al. The deep inspiration breath-hold technique in the treatment of inoperable nonsmall-cell lung cancer. Int J Radiat Oncol Biol Phys. 48:81–7. 2000.15. Kubo HD, Hill BC. Respiration gated radiotherapy treatment: A technical study. Phys Med Biol. 41:83–91. 1996.
Article16. Li XA, Stepaniak C, Gore E. Technical and dosimetric aspects of respiratory gating using a pressure-sensor motion monitoring system. Med Phys. 33:145–54. 2006.
Article17. Keall PJ, Mageras GS, Balter JM, et al. The management of respiratory motion in radiation oncology report of AAPM TG 76. Med Phys. 33(10):3874–3900. 2006.18. Song JY, Nah BS, Jung WK, et al. Development of error analysis program for phase – based respiratory gating radiation therapy. Korean J Med Physics. 17(3):136–143. 2006.19. Lim S, Park S, Ahn SD, et al. Guiding curve based on the normal breathing as monitored by thermocouple for regular breathing. Med Phys. 34:4514–4518. 2007.
Article20. Ali I, Lovelock D, Kang H, et al. Extraction of internal andexternal marker 3D-motion in liver patients with compression belt using kV cone-beam radiographic projections. Med Phys. 34:2392. 2007.21. Zhang T, Keller H, O'Brien MJ, Mackie TR, Paliwal B. Application of the spirometer in respiratory gated radiotherapy. Med Phys. 30:3165–3172. 2003.
Article22. Casamassima F, Cavedon C, Francescon P, et al. Use of motion tracking in stereotactic body radiotherapy: Evaluation of uncertainty in off-target dose distribution and optimization strategies. Acta Oncological. 45:943–947. 2006.
Article23. Kuo JS, Yu C, Petrovich Z, et al. The CyberKnife stereotactic radiosurgery system: description, installation and an initial evaluation of use and functionality. Neurosurgery. 52:1235–1239. 2003.
Article24. Kang YN, Jang JS, Choi BO, et al. Evaluation of the Gating System Using Moving Phantom in CyberKnife. World Congress on Medical Physics and Biomedical Engineering. 2006. Seoul, pp.3446.25. Schweikard A, Glosser G, Bodduluri M, et al. Robotic motion compensation for respiratory movement during radiosurgery. Comput Aided Surg 5, 263–277 490 (. 2000.26. Ozhasoqiu C, Saw CB, Chen H, et al. Synchrony-CyberKnife respiratory compensation technology. Med Dosim. 33(2):117–123. 2008.27. Ozhasoqiu C, Murphy MJ, Glosser G. Real time tracking of the tumor volume in precision radiotherapy and body radiosurgery-A novel approach to compensate for respiratory motion. Com Ass Radio Surg 691–696 (. 2000.28. Shin EH, Park HC, Han YY, et al. Efficacy of a Respiratory Training System on the Regularity of Breathing. J Korean Radiol Soc. 26(3):181–188. 2008.
Article29. Kang SH, Yoon JW, Kim TH, Suh TS. Development of Respiratory Training System Using Individual Characteristic Guiding Waveform. Korean J Med Physics. 23(1):1–7. 2012.
Article30. Venkat RB, Keall P, Sawant A, George R. Respiratory training using audio visual biofeedback. Med Phys. 34:2370. 2007.31. Kini VR, Vedam SS, Keall PJ, et al. Patient training in respiratory-gated radiotherapy. Med Dosim. 28:7–11. 2003.
Article32. Rohini G, Thedore D C, Sastry S V, et al. Audiovisual biofeedback for respiratory-gated radiotherapy: Impact of audio instruction and audio-visual biofeedback on respiratory radiotherapy. Int J Radiation Oncology Biol Phys. 65(3):924–933. 2006.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stereotactic Body Radiotherapy for Early Stage Lung Cancer
- Current status of stereotactic body radiotherapy for the treatment of hepatocellular carcinoma
- Stereotactic Body Radiation Therapy
- Stereotactic Body Radiation Therapy for Hepatocellular Carcinoma
- Stereotactic Body Radiotherapy: Does It Have a Role in Management of Hepatocellular Carcinoma?