Korean J Urol.
2011 Mar;52(3):216-220.
Value and Safety of Midazolam Anesthesia during Transrectal Ultrasound-Guided Prostate Biopsy
- Affiliations
-
- 1Department of Urology, Soonchunhyang University College of Medicine, Seoul, Korea. yssong@schmc.ac.kr
- 2Department of Urology, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Urology, Soonchunhyang University College of Medicine, Cheonan, Korea.
Abstract
- PURPOSE
Although transrectal ultrasound-guided prostate biopsy is useful for diagnosing prostate cancer, it is a painful procedure. There are many methods for providing pain relief and for treating discomfort during the procedure, but occasionally these are reported to be of limited use. We aimed to evaluate the value and safety of midazolam-induced anesthetic transrectal ultrasound-guided prostate biopsy.
MATERIALS AND METHODS
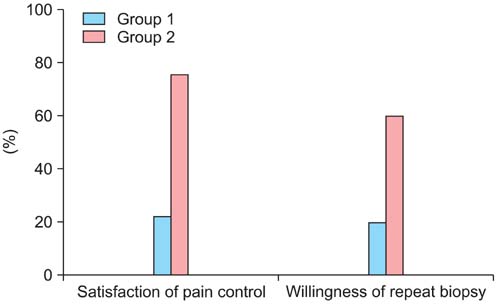
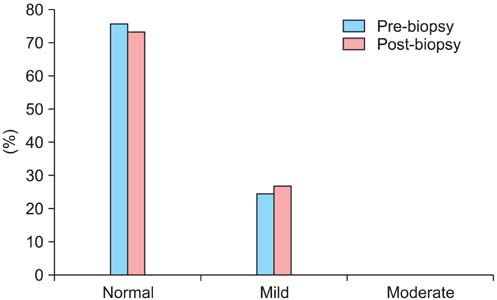
From August 2008 to December 2009, 104 male patients, who were examined with transrectal ultrasound-guided prostate 12-core biopsy, were randomly assigned to two groups. Group 1 (n=51) received ketorolac (Tarasyn(R)) 30 mg. Group 2 (n=53) was treated with midazolam (Dormicum(R)) 3 mg, which was increased to 5 mg if necessary. Immediately after the procedure, the patients were asked to rate their comfort level by using a 10-point visual analog self-assessment pain scale.
RESULTS
The pain scale in group 2 was significantly lower than that in group 1 (p<0.05). The patients assigned to group 2 experienced no side-effects from midazolam and were more satisfied than the patients in group 1 (p<0.05).
CONCLUSIONS
Midazolam anesthesia relieves pain effectively, and the patient's satisfaction is better than with conventional transrectal ultrasound-guided prostate biopsy. Midazolam-induced anesthetic transrectal ultrasound-guided prostate biopsy is useful and safe.
Keyword
MeSH Terms
Figure
Reference
-
1. Ross WA. Premedication for upper gastrointestinal endoscopy. Gastrointest Endosc. 1989. 35:120–126.2. Whitwam JG, Al-Khudhairi D, McCloy RF. Comparison of midazolam and diazepam in doses of comparable potency during gastroscopy. Br J Anaesth. 1983. 55:773–777.3. Hanno PM, Wein AJ. Anesthetic techniques for cystoscopy in men. J Urol. 1983. 130:1070–1072.4. Forrest P, Galletly DC. Comparison of propofol and antagonised midazolam anaesthesia for day-case surgery. Anaesth Intensive Care. 1987. 15:394–401.5. Johnson EW. Visual analog scale (VAS). Am J Phys Med Rehabil. 2001. 80:717.6. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975. 12:189–198.7. Kang Y, Na DL, Hahn S. Validity study on the Korean mini-mental state examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997. 15:300–307.8. Collins GN, Lloyd SN, Hehir M, McKelvie GB. Multiple transrectal ultrasound-guided prostatic biopsies--true morbidity and patient acceptance. Br J Urol. 1993. 71:460–463.9. Djavan B, Waldert M, Zlotta A, Dobronski P, Seitz C, Remzi M, et al. Safety and morbidity of first and repeat transrectal ultrasound guided prostate needle biopsies: results of a prospective European prostate cancer detection study. J Urol. 2001. 166:856–860.10. Gerecke M. Chemical structure and properties of midazolam compared with other benzodiazepines. Br J Clin Pharmacol. 1983. 16:Suppl 1. 11S–16S.11. Pieri L. Preclinical pharmacology of midazolam. Br J Clin Pharmacol. 1983. 16:Suppl 1. 17S–27S.12. Reves JG, Fragen RJ, Vinik HR, Greenblatt DJ. Midazolam: pharmacology and uses. Anesthesiology. 1985. 62:310–324.13. Kanto JH. Midazolam: the first water-soluble benzodiazepine. Pharmacology, pharmacokinetics and effcacy in insomnia and anesthesia. Pharmacotherapy. 1985. 5:138–155.14. Amrein R, Hetzel W. Pharmacology of drugs frequently used in ICUs: midazolam and flumazenil. Intensive Care Med. 1991. 17:Suppl 1. S1–S10.15. Greenblatt DJ, Shader RI, Abernethy DR. Drug therapy. Current status of benzodiazepines. N Engl J Med. 1983. 309:410–416.16. Study RE, Barker JL. Cellular mechanisms of benzodiazepine action. JAMA. 1982. 247:2147–2151.17. Dundee JW, Wilson DB. Amnesic action of midazolam. Anaesthesia. 1980. 35:459–461.18. Koht A, Moss JI. Does midazolam cause retrograde amnesia, and can flumazenil reverse that amnesia? Anesth Analg. 1997. 85:211–212.19. Twersky RS, Hartung J, Berger BJ, McClain J, Beaton C. Midazolam enhances anterograde but not retrograde amnesia in pediatric patients. Anesthesiology. 1993. 78:51–55.20. Bulach R, Myles PS, Russnak M. Double-blind randomized controlled trial to determine extent of amnesia with midazolam given immediately before general anaesthesia. Br J Anaesth. 2005. 94:300–305.21. Lauven PM, Kulka PJ. Anaesthesia techniques for midazolam and flumazenil--an overview. Acta Anaesthesiol Scand Suppl. 1990. 92:84–89.22. Desgrandchamps F, Meria P, Irani J, Desgrippes A, Teillac P, Le Duc A. The rectal administration of lidocaine gel and tolerance of tansrectal ultrasonography-guided biopsy of the prostate: a prospective randomized placebo-controlled study. BJU Int. 1999. 83:1007–1009.23. Wu CL, Carter HB, Naqibuddin M, Fleisher LA. Effect of local anesthetics on patient recovery after transrectal biopsy. Urology. 2001. 57:925–929.24. Leibovici D, Zisman A, Siegel YI, Sella A, Kleinmann J, Lindner A. Local anaesthesia for prostate biopsy by periprostatic lidocaine injection: a double-blind placebo controlled study. J Urol. 2002. 167:563–565.25. Irani J, Fournier F, Bon D, Gremmo E, Dóre B, Aubert J. Patient tolerance of transrectal ultrasound-guided biopsy of the prostate. Br J Urol. 1997. 79:608–610.26. Turgut AT, Ergun E, Koşar U, Koşar P, Ozcan A. Sedation as an alternative method to lessen patient discomfort due to transrectal ultrasonography-guided prostate biopsy. Eur J Radiol. 2006. 57:148–153.27. Peters JL, Thompson AC, McNicholas TA, Hines JE, Hanbury DC, Boustead GB. Increased patient satisfaction from transrectal ultrasonography and biopsy under sedation. BJU Int. 2001. 87:827–830.28. Forster A, Gardaz JP, Suter PM, Gemperle M. I.V. midazolam as an induction agent for anaesthesia a study in volunteers. Br J Anaesth. 1980. 52:907–911.29. Ginsberg GG, Lewis JH, Gallagher JE, Fleischer DE, al-Kawas FH, Nguyen CC, et al. Diazepam versus midazolam for colonoscopy: a prospective evaluation of predicted versus actual dosing requirements. Gastrointest Endosc. 1992. 38:651–656.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pain during Transrectal Ultrasound-Guided Prostate Biopsy and the Role of Periprostatic Nerve Block: What Radiologists Should Know
- Efficacy and Safety of Intravenous Propofol Anesthesia during Transrectal Ultrasound-Guided Prostate Biopsy
- Transrectal Ultrasound Guided Prostate Biopsy: Current Status and Controversy
- Prostate Cancer Detection by Transrectal Ultrasound Guided Prostate Biopsy: Urology versus Radiology at a Single Academic Institution
- Effect of Periprostatic Nerve Blockade for Transrectal Ultrasound Guided Biopsy of the Prostate