Korean J Urol.
2012 Aug;53(8):524-530.
Preoperative Factors Predictive of Continence Recovery after Radical Retropubic Prostatectomy
- Affiliations
-
- 1Department of Urology, Kyung Hee University School of Medicine, Seoul, Korea. sgchang@urology.or.kr
- 2Department of Radiology, Kyung Hee University School of Medicine, Seoul, Korea.
Abstract
- PURPOSE
We assessed the factors predictive of continence recovery after radical retropubic prostatectomy performed by use a single operative technique by a single surgeon.
MATERIALS AND METHODS
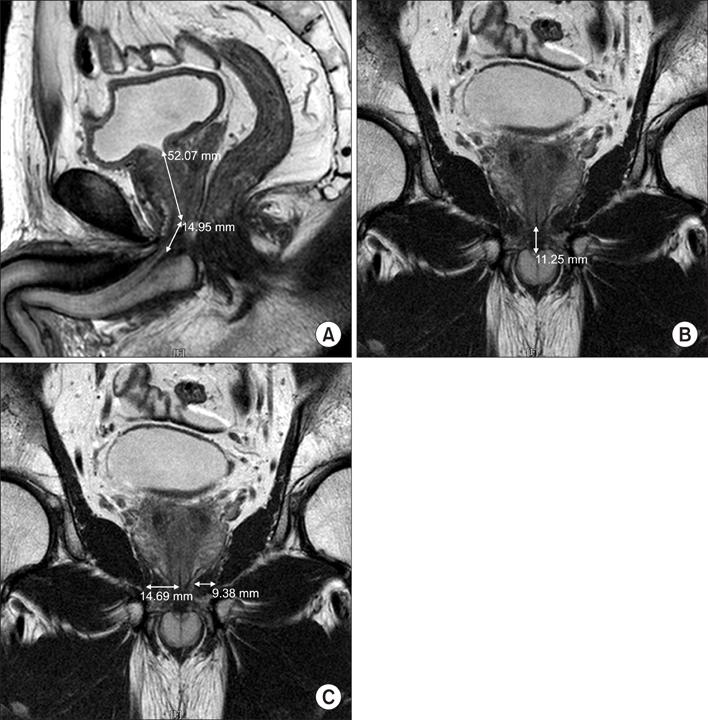
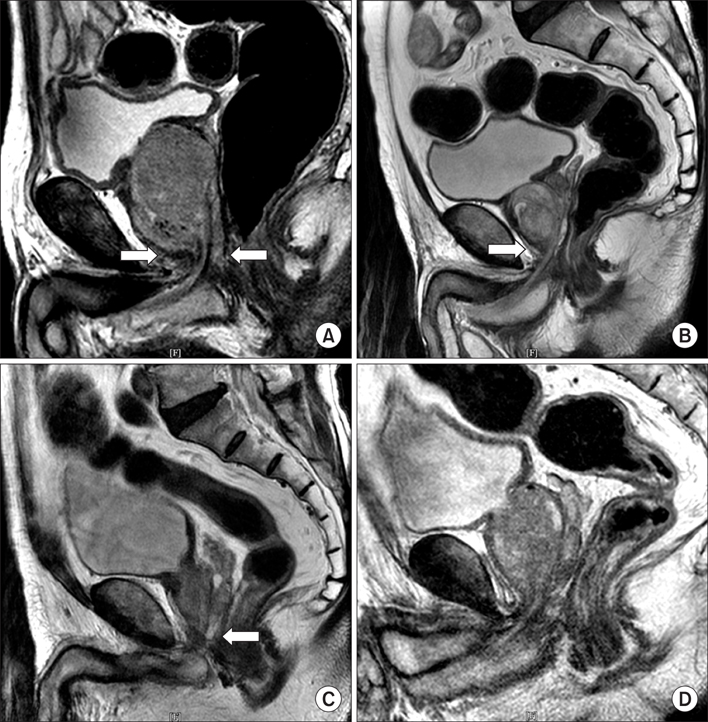
Preoperative factors, including age, body mass index (BMI), prostate volume, prostate-specific antigen level, and anatomical information from preoperative magnetic resonance imaging (MRI), such as membranous urethral length, thickness of the levator ani muscle, and urogenital diaphragm, were evaluated in 94 consecutive patients who underwent radical retropubic prostatectomy between April 2005 and October 2010. Patients were also categorized into four different groups according to the overlying pattern of the prostatic apex and the membranous urethra. Continence status was evaluated by direct patient questioning at 12 months after the operation.
RESULTS
The overall continence rate at 12 months after the operation was 79.8%. In the age- and BMI-adjusted logistic regression analysis, the membranous urethral length and the overlying pattern of the prostatic apex were significant predictive factors of the continence rate at 12 months after the operation (p=0.006 and p=0.007, respectively). Other predictive factors were not contributory. Patients with no overlapping observed between the prostatic apex and membranous urethra had longer membranous urethral lengths (14.24+/-2.73 mm) and higher rates of recovery of continence compared with other groups.
CONCLUSIONS
Membranous urethral length and shape of the prostatic apex as assessed by preoperative MRI are significantly associated with recovery of urinary continence after radical retropubic prostatectomy.
MeSH Terms
Figure
Reference
-
1. Henry RY, O'Mahony D. Treatment of prostate cancer. J Clin Pharm Ther. 1999. 24:93–102.2. Catalona WJ, Carvalhal GF, Mager DE, Smith DS. Potency, continence and complication rates in 1,870 consecutive radical retropubic prostatectomies. J Urol. 1999. 162:433–438.3. Steiner MS, Morton RA, Walsh PC. Impact of anatomical radical prostatectomy on urinary continence. J Urol. 1991. 145:512–514.4. Eastham JA, Kattan MW, Rogers E, Goad JR, Ohori M, Boone TB, et al. Risk factors for urinary incontinence after radical prostatectomy. J Urol. 1996. 156:1707–1713.5. Graefen M, Walz J, Huland H. Open retropubic nerve-sparing radical prostatectomy. Eur Urol. 2006. 49:38–48.6. Coughlin G, Palmer KJ, Shah K, Patel VR. Robotic-assisted radical prostatectomy: functional outcomes. Arch Esp Urol. 2007. 60:408–418.7. Mottrie A, Van Migem P, De Naeyer G, Schatteman P, Carpentier P, Fonteyne E. Robot-assisted laparoscopic radical prostatectomy: oncologic and functional results of 184 cases. Eur Urol. 2007. 52:746–750.8. Lee SE, Byun SS, Lee HJ, Song SH, Chang IH, Kim YJ, et al. Impact of variations in prostatic apex shape on early recovery of urinary continence after radical retropubic prostatectomy. Urology. 2006. 68:137–141.9. Song C, Doo CK, Hong JH, Choo MS, Kim CS, Ahn H. Relationship between the integrity of the pelvic floor muscles and early recovery of continence after radical prostatectomy. J Urol. 2007. 178:208–211.10. Coakley FV, Eberhardt S, Kattan MW, Wei DC, Scardino PT, Hricak H. Urinary continence after radical retropubic prostatectomy: relationship with membranous urethral length on preoperative endorectal magnetic resonance imaging. J Urol. 2002. 168:1032–1035.11. Wolin KY, Luly J, Sutcliffe S, Andriole GL, Kibel AS. Risk of urinary incontinence following prostatectomy: the role of physical activity and obesity. J Urol. 2010. 183:629–633.12. Paparel P, Akin O, Sandhu JS, Otero JR, Serio AM, Scardino PT, et al. Recovery of urinary continence after radical prostatectomy: association with urethral length and urethral fibrosis measured by preoperative and postoperative endorectal magnetic resonance imaging. Eur Urol. 2009. 55:629–637.13. Majoros A, Bach D, Keszthelyi A, Hamvas A, Mayer P, Riesz P, et al. Analysis of risk factors for urinary incontinence after radical prostatectomy. Urol Int. 2007. 78:202–207.14. Sacco E, Prayer-Galetti T, Pinto F, Fracalanza S, Betto G, Pagano F, et al. Urinary incontinence after radical prostatectomy: incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up. BJU Int. 2006. 97:1234–1241.15. Myers RP, Cahill DR, Devine RM, King BF. Anatomy of radical prostatectomy as defined by magnetic resonance imaging. J Urol. 1998. 159:2148–2158.16. Johansson E, Steineck G, Holmberg L, Johansson JE, Nyberg T, Ruutu M, et al. Long-term quality-of-life outcomes after radical prostatectomy or watchful waiting: the Scandinavian Prostate Cancer Group-4 randomised trial. Lancet Oncol. 2011. 12:891–899.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Retrograde Urethrography as a Predictor of Early Recovery of Urinary Continence after Radical Retropubic Prostatectomy
- Comparison of Continence Recovery Between Robot-Assisted Laparoscopic Prostatectomy and Open Radical Retropubic Prostatectomy: A Single Surgeon Experience
- Effect of Nerve-Sparing Radical Prostatectomy on Urinary Continence in Patients With Preoperative Erectile Dysfunction
- Association between cystographic anastomotic urinary leakage following retropubic radical prostatectomy and early urinary incontinence
- Initial Experience of Three Cases of Radical Retropubic Prostatectomy