Korean J Urol.
2012 May;53(5):330-334.
The Prevalence and Characteristic Differences in Prostatic Calcification between Health Promotion Center and Urology Department Outpatients
- Affiliations
-
- 1Department of Urology, Yeouido St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. cyh0831@catholic.ac.kr
- 2Department of Urology, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea.
Abstract
- PURPOSE
We evaluated the differences in calculi characteristics and their prevalence according to the presence of lower urinary tract symptoms between adult patients examined at the Urology Department and those examined at the Health Promotion Center (HPC).
MATERIALS AND METHODS
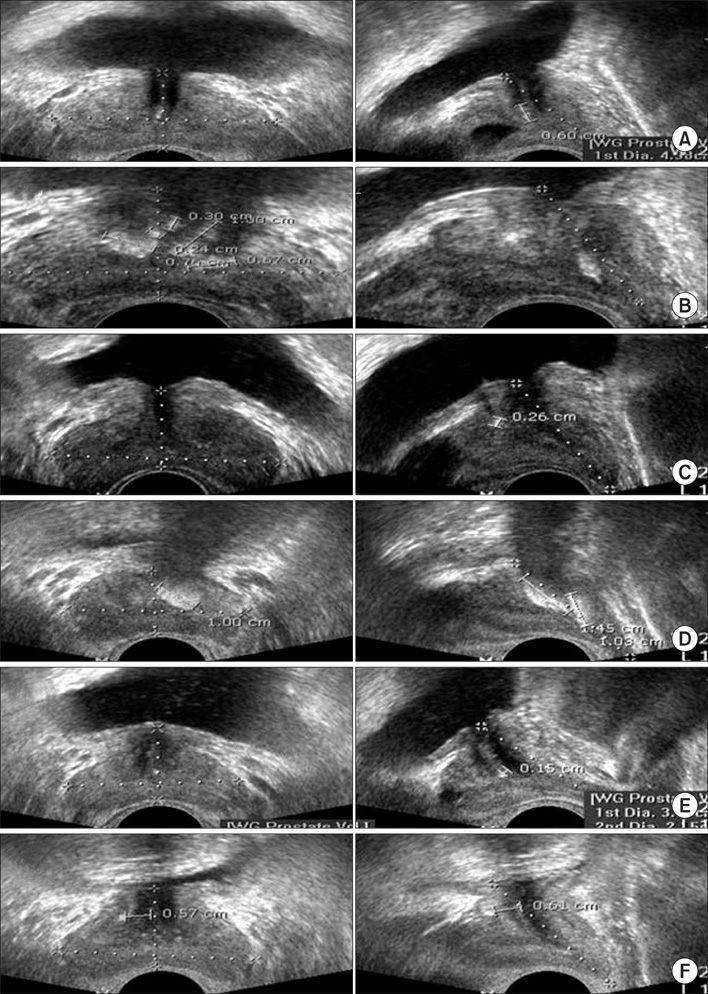
The prevalence of prostatic calcification, characteristics of calculi (number, size, and location), and differences in lower urinary tract symptoms were compared and analyzed for 479 subjects who underwent transrectal ultrasonography at the HPC and the Urology Outpatients Department at our hospital from October 2009 to October 2010.
RESULTS
Of 479 subjects, 268 patients were examined at the HPC, and 211 were examined at the Urology Outpatients Department. Between the two groups, age, prostate-specific antigen levels, prostate volume transrectal ultrasonography, International Prostate Symptom Score (total, voiding, and storage), quality of life, and the prostatic calcification rate were significantly higher in the patients who visited the Urology Outpatients Department. The prevalence of prostatic calcification was 41.5% (199/479), with 36.1% (97/268) from the HPC and 48.3% (102/211) from the Urology Outpatients Department. When the characteristics of prostatic calcification were compared, there were no significant differences in the appearance, size, or location of the calculi between the two groups.
CONCLUSIONS
The prevalence of prostatic calcification was high in patients complaining of lower urinary tract symptoms; however, there were no significant differences in the characteristics of the calculi. This finding leads us to believe that prostatic calcification can aggravate lower urinary tract symptoms but does not result in differences according to the number, size, or appearance of the calculi.
Keyword
MeSH Terms
Figure
Reference
-
1. Geramoutsos I, Gyftopoulos K, Perimenis P, Thanou V, Liagka D, Siamblis D, et al. Clinical correlation of prostatic lithiasis with chronic pelvic pain syndromes in young adults. Eur Urol. 2004. 45:333–337.2. Park SW, Nam JK, Lee SD, Chung MK. Are prostatic calculi independent predictive factors of lower urinary tract symptoms? Asian J Androl. 2010. 12:221–226.3. Fox M. The natural history and significance of stone formation in the prostate gland. J Urol. 1963. 89:716–727.4. Sondergaard G, Vetner M, Christensen PO. Prostatic calculi. Acta Pathol Microbiol Immunol Scand A. 1987. 95:141–145.5. Horio Y. On the morphological alteration of the prostate gland in aging. I. A histopathologic study of the prostate gland and the testis in aging and the correlation of their senile changes. Nihon Hinyokika Gakkai Zasshi. 1967. 58:783–813.6. Leader AJ, Queen DM. Prostatic calculous disease. J Urol. 1958. 80:142–146.7. Klimas R, Bennett B, Gardner WA Jr. Prostatic calculi: a review. Prostate. 1985. 7:91–96.8. Ho KL, Segura JW. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Lower urinary tract calculi. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;2663–2673.9. Kirby RS, Lowe D, Bultitude MI, Shuttleworth KE. Intra-prostatic urinary reflux: an aetiological factor in abacterial prostatitis. Br J Urol. 1982. 54:729–731.10. Shoskes DA, Lee CT, Murphy D, Kefer J, Wood HM. Incidence and significance of prostatic stones in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2007. 70:235–238.11. Kim SG, Han WC, Jeong HJ, Rim JS. The influence of prostatic calcification and lymphocyte infiltration on the result of TURP in patients with benign prostatic hyperplasia. Korean J Urol. 2003. 44:82–86.12. Cha WH, Kim KH, Seo YJ. The effect of periurethral prostatic calculi on lower urinary tract symptoms in benign prostatic hyperplasia. Korean J Urol. 2008. 49:237–241.13. Peeling WB, Griffiths GJ. Imaging of the prostate by ultrasound. J Urol. 1984. 132:217–224.14. Kim WB, Doo SW, Yang WJ, Song YS. Influence of prostatic calculi on lower urinary tract symptoms in middle-aged men. Urology. 2011. 78:447–449.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Seropositivity to Trichomonas vaginalis between Men with Prostatic Tumor and Normal Men
- Imaging of tbe Prostatic Carcinoma and Benign Prostatic Hyperplasia by Transrectal Ultrasound
- The Correlation between Metabolic Syndrome and the Prostate Volume
- New Thresholds for Prostate-specific Antigen Velocity for Prostate Cancer Screening in Korean Patients Younger than 60 Years Old
- Gender Differences in Health Status, Health Behavior and Disease Prevalence of Multi-cultural Family