Korean J Urol.
2012 Jun;53(6):401-404.
Use of Cystoscopic Tattooing in Laparoscopic Partial Cystectomy
- Affiliations
-
- 1Department of Urology, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea. ysurol@schmc.ac.kr
Abstract
- PURPOSE
During laparoscopic partial cystectomy (LPC), lesion identification is essential to help to determine the appropriate bladder incisions required to maintain adequate resection margins. The inability to use tactile senses makes it difficult for surgeons to locate lesions during laparoscopic surgery. Endoscopic India ink marking techniques are often used in laparoscopic gastroenterological surgery. We present our experience with performing LPC with India ink during the surgical resection of various bladder lesions.
MATERIALS AND METHODS
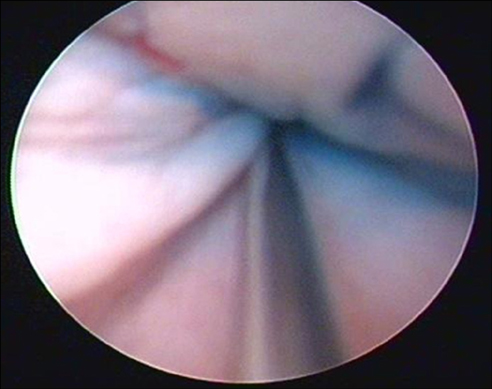
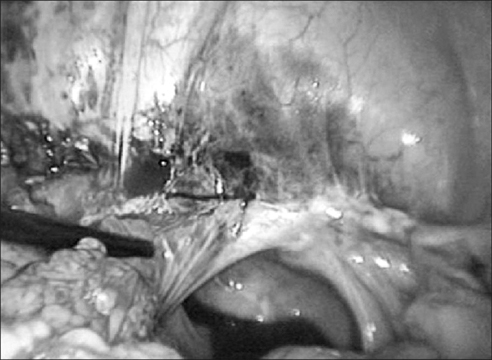
LPC with cystoscopic fine needle tattooing was performed on 10 patients at our institute. Tattooing was performed at 1- to 2-cm intervals approximately 1 cm away from the outer margin of the lesion with enough depth (the deep muscle layer) under cystoscopic guidance. LPC was performed by the transperitoneal approach. The clinical courses and pathologic results were analyzed.
RESULTS
All LPC with cystoscopic tattooing cases were performed successfully. The mean patient age was 39.1 years. The mean operative time was 130.5 minutes, and the mean estimated blood loss was 93 ml. The mean hospital stay was 13.1 days, and the mean duration of indwelling Foley catheterization was 10.7 days. There were no significant intraoperative or postoperative complications except 1 case of delayed urinary leak and 1 case of delayed wound healing. The pathological diagnosis included 1 urachal cancer, 1 urachal remnant, 4 urachal cysts, 2 pheochromocytomas, and 2 inflammatory masses. All specimens showed adequate surgical margins.
CONCLUSIONS
Cystoscopic tattooing in LPC is a simple and effective technique to assist in locating pathological bladder lesions intraoperatively. This technique can help to determine appropriate resection margins during LPC without incurring additional complicated procedures.
Keyword
MeSH Terms
Figure
Reference
-
1. Sweeney P, Kursh ED, Resnick MI. Partial cystectomy. Urol Clin North Am. 1992. 19:701–711.2. Nezhat CR, Nezhat FR. Laparoscopic segmental bladder resection for endometriosis: a report of two cases. Obstet Gynecol. 1993. 81(5 Pt 2):882–884.3. Mariano MB, Tefilli MV. Laparoscopic partial cystectomy in bladder cancer--initial experience. Int Braz J Urol. 2004. 30:192–198.4. Colombo JR Jr, Desai M, Canes D, Frota R, Haber GP, Moinzadeh A, et al. Laparoscopic partial cystectomy for urachal and bladder cancer. Clinics (Sao Paulo). 2008. 63:731–734.5. Feingold DL, Addona T, Forde KA, Arnell TD, Carter JJ, Huang EH, et al. Safety and reliability of tattooing colorectal neoplasms prior to laparoscopic resection. J Gastrointest Surg. 2004. 8:543–546.6. McArthur CS, Roayaie S, Waye JD. Safety of preoperation endoscopic tattoo with india ink for identification of colonic lesions. Surg Endosc. 1999. 13:397–400.7. Ferzli G, Wenof M, Giannakakos A, Raboy A, Albert P. Laparoscopic partial cystectomy for vesical endometrioma. J Laparoendosc Surg. 1993. 3:161–165.8. Nezhat C, Nezhat F, Nezhat CH, Nasserbakht F, Rosati M, Seidman DS. Urinary tract endometriosis treated by laparoscopy. Fertil Steril. 1996. 66:920–924.9. Kozlowski PM, Mihm F, Winfield HN. Laparoscopic management of bladder pheochromocytoma. Urology. 2001. 57:365.10. Tai HC, Chung SD, Wang SM, Chueh SC, Yu HJ. Laparoscopic partial cystectomy for various bladder pathologies. BJU Int. 2007. 100:382–385.11. Geol H, Kim DW, Kim TH, Seong YK, Cho WY, Kim SD, et al. Laparoscopic partial cystectomy for schwannoma of urinary bladder: case report. J Endourol. 2005. 19:303–306.12. Allam ME, Mehta D, Zelen J, Fogler R. Posterior wall gastric leiomyoma: endoscopic tattooing facilitates laparoscopic resection. JSLS. 1998. 2:83–84.13. Aboosy N, Mulder CJ, Berends FJ, Meijer JW, Sorge AA. Endoscopic tattoo of the colon might be standardized to locate tumors intraoperatively. Rom J Gastroenterol. 2005. 14:245–248.14. Abdel-Hakim AM, El-Feel A, Abouel-Fettouh H, Saad I. Laparoscopic vesical diverticulectomy. J Endourol. 2007. 21:85–89.15. Ponsky JL, King JF. Endoscopic marking of colonic lesions. Gastrointest Endosc. 1975. 22:42–43.16. Askin MP, Waye JD, Fiedler L, Harpaz N. Tattoo of colonic neoplasms in 113 patients with a new sterile carbon compound. Gastrointest Endosc. 2002. 56:339–342.17. Arteaga-Gonzalez I, Martín-Malagon A, Fernandez EM, Arranz-Duran J, Parra-Blanco A, Nicolas-Perez D, et al. The use of preoperative endoscopic tattooing in laparoscopic colorectal cancer surgery for endoscopically advanced tumors: a prospective comparative clinical study. World J Surg. 2006. 30:605–611.18. Lane KL, Vallera R, Washington K, Gottfried MR. Endoscopic tattoo agents in the colon. Tissue responses and clinical implications. Am J Surg Pathol. 1996. 20:1266–1270.19. Hyman N, Waye JD. Endoscopic four quadrant tattoo for the identification of colonic lesions at surgery. Gastrointest Endosc. 1991. 37:56–58.20. Nizam R, Siddiqi N, Landas SK, Kaplan DS, Holtzapple PG. Colonic tattooing with India ink: benefits, risks, and alternatives. Am J Gastroenterol. 1996. 91:1804–1808.21. Shatz BA, Weinstock LB, Swanson PE, Thyssen EP. Long-term safety of India ink tattoos in the colon. Gastrointest Endosc. 1997. 45:153–156.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A successful case of laparoscopic partial cystectomy for bladder endometriosis
- Laparoscopic Partial Cystectomy for Adenocarcinoma of the Bladder
- A Technique of Partial Cystectomy for Carcinoma
- Removal of foreign bodies embedded in the urinary bladder wall by a combination of laparoscopy and carbon dioxide cystoscopic assistance: Case report and literature review
- Inflammatory Myofibroblastic Tumor of the Urinary Bladder Managed by Laparoscopic Partial Cystectomy