Korean J Urol.
2010 Apr;51(4):266-270.
The Effect of Intraprostatic Chronic Inflammation on Benign Prostatic Hyperplasia Treatment
- Affiliations
-
- 1Department of Urology, Keimyung University School of Medicine, Daegu, Korea. cikim@dsmc.or.kr
- 2Department of Pathology, Keimyung University School of Medicine, Daegu, Korea.
Abstract
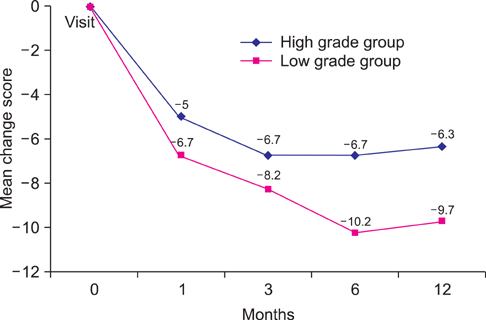
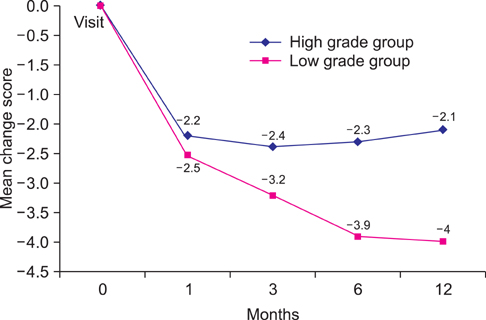
- PURPOSE
Asymptomatic chronic inflammation of the prostate is a common finding in benign prostatic hyperplasia (BPH). We investigated how the chronic inflammation affects medical treatment for BPH. MATERIALS AND METHODS: One pathologist reviewed the chronic inflammation of 82 BPH patients who underwent transrectal ultrasonography (TRUS)-guided needle biopsy. The extent of chronic inflammation was classified into 4 grades, categorized into two groups: the low-grade group and the high-grade group. We compared total, voiding, and storage International Prostate Symptom Score (IPSS) and quality of life (QoL) between the groups at baseline and 1, 3, 6, and 12 months after medical treatment for BPH. RESULTS: There were no significant differences in total IPSS or QoL between the groups during the follow-up period. The low-grade group showed continuous improvement of storage symptoms until 12 months; however, the high-grade group showed improvement until 3 months. Maximal improvements of QoL were observed at 6 months in the high-grade group and at 3 months in the low-grade group. There was no episode of surgery in the low-grade group, but four patients in the high-grade group (9.1%) underwent surgical treatment due to acute urinary retention or insufficient therapeutic response. CONCLUSIONS: Although there was no statistical significance, improvements in IPSS were higher and lasted longer in the low-grade group. We might suggest medical treatment for intraprostatic chronic inflammation in BPH patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Djavan B, Fong YK, Harik M, Milani S, Reissigl A, Chaudry A, et al. Longitudinal study of men with mild symptoms of bladder outlet obstruction treated with watchful waiting for four years. Urology. 2004. 64:1144–1148.2. Crawford ED, Wilson SS, McConnell JD, Slawin KM, Lieber MC, Smith JA, et al. Baseline factors as predictors of clinical progression of benign prostatic hyperplasia in men treated with placebo. J Urol. 2006. 175:1422–1426.3. Roehrborn CG, Kaplan SA, Noble WD, Lucia MS, Slawin KM, McVary KT, et al. The impact of acute or chronic inflammation in baseline biopsy on the risk of clinical progression of BPH: results from the MTOPS study. J Urol. 2005. 173:Suppl. 346. abstract 1277.4. Mishra VC, Allen DJ, Nicolaou C, Sharif H, Hudd C, Karim OM, et al. Does intraprostatic inflammation have a role in the pathogenesis and progression of benign prostatic hyperplasia? BJU Int. 2007. 100:327–331.5. Kefi A, Koseoglu H, Celebi I, Yorukoglu K, Esen A. Relation between acute urinary retention, chronic prostatic inflammation and accompanying elevated prostate-specific antigen. Scand J Urol Nephrol. 2006. 40:155–160.6. Tuncel A, Uzun B, Eruyar T, Karabulut E, Seckin S, Atan A. Do prostatic infarction, prostatic inflammation and prostate morphology play a role in acute urinary retention? Eur Urol. 2005. 48:277–283.7. Ha JY, Kwak DY, Chang HS, Park CH, Kwon SY, Kim CI. Relationship between acute urinary retention and intraprostatic inflammation in benign prostatic hyperplasia. Korean J Urol. 2008. 49:1081–1086.8. Irani J, Levillain P, Goujon JM, Bon D, Dore B, Aubert J. Inflammation in benign prostatic hyperplasia: correlation with prostate specific antigen value. J Urol. 1997. 157:1301–1303.9. Kohnen PW, Drach GW. Patterns of inflammation in prostatic hyperplasia: a histologic and bacteriologic study. J Urol. 1979. 121:755–760.10. Nickel JC, Roehrborn CG, O'Leary MP, Bostwick DG, Somerville MC, Rittmaster RS. The relationship between prostate inflammation and lower urinary tract symptoms: examination of baseline data from the REDUCE trial. Eur Urol. 2008. 54:1379–1384.11. Nickel JC. Prostatic inflammation in benign prostatic hyperplasia-the third component? Can J Urol. 1994. 1:1–4.12. Kang TW, Oh BR, Kim KW, Min KD, Kwon DD, Ryu SB. Clinical significance of prostatitis in patients with benign prostatic hyperplasia. Korean J Urol. 2003. 44:278–282.13. Schaeffer AJ. Evaluation of the cytokines in genital secretions of patients with chronic prostatitis. J Urol. 2005. 173:844–845.14. Miller LJ, Fischer KA, Goralnick SJ, Litt M, Burleson JA, Albertsen P, et al. Nerve growth factor and chronic prostatitis/ chronic pelvic pain syndrome. Urology. 2002. 59:603–608.15. Orhan I, Onur R, Ilhan N, Ardiçoglu A. Seminal plasma cytokine levels in the diagnosis of chronic pelvic pain syndrome. Int J Urol. 2001. 8:495–499.16. Nickel JC, Downey J, Young I, Boag S. Asymptomatic inflammation and/or infection in benign prostatic hyperplasia. BJU Int. 1999. 84:976–981.17. Collins MM, Meigs JB, Barry MJ, Walker Corkery E, Giovannucci E, Kawachi I. Prevalence and correlates of prostatitis in the health professionals follow-up study cohort. J Urol. 2002. 167:1363–1366.18. Nickel JC. Inflammation and benign prostatic hyperplasia. Urol Clin North Am. 2008. 35:109–115.19. Ozdemir I, Bozkurt O, Demir O, Aslan G, Esen AA. Combination therapy with doxazosin and tenoxicam for the management of lower urinary tract symptoms. Urology. 2009. 74:431–435.20. Di Silverio F, Bosman C, Salvatori M, Albanesi L, Proietti Pannunzi L, Ciccariello M, et al. Combination therapy with rofecoxib and finasteride in the treatment of men with lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Eur Urol. 2005. 47:72–78.21. Minnery CH, Getzenberg RH. Benign prostatic hyperplasia cell line viability and modulation of jm-27 by doxazosin and ibuprofen. J Urol. 2005. 174:375–379.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Intraprostatic Inflammation in Patients with Lower Urinary Tract Symptoms Suggestive of Benign Prostatic Hyperplasia
- Initial experience of 5 cases of intraprostatic spiral(PROSTAKA(TH))
- Relationship between Acute Urinary Retention and Intraprostatic Inflammation in Benign Prostatic Hyperplasia
- Indwelling of an intraprostatic stent(prostakath/TM and nissenkorn catheter): possibilities as a definitive management for benign prostatic hyperplasia
- Insertion of intraprostatic spiral(urospiral@) in high risk patients with benign prostatic hyperplasia