Korean J Urol.
2010 Apr;51(4):245-249.
Renal Function Recovery in Donors and Recipients after Live Donor Nephrectomy: Hand-Assisted Laparoscopic vs. Open Procedures
- Affiliations
-
- 1Department of Urology, School of Medicine, Kyungpook National University, Daegu, Korea. tgkwon@knu.ac.kr
Abstract
- PURPOSE
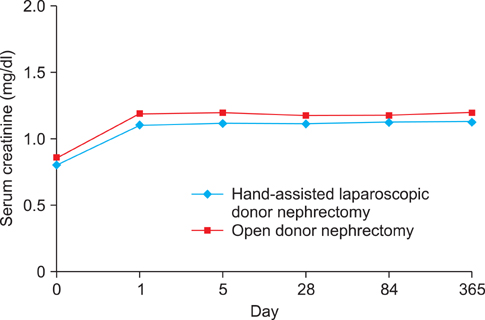
Laparoscopic donor nephrectomy is associated with less postoperative pain and faster recovery times in living kidney donors. However, pneumoperitoneum, which is required in laparoscopic donor nephrectomy, can result in adverse effects on renal function in donors and recipients. We compared renal function in donors and recipients after hand-assisted laparoscopic donor nephrectomy (HALDN) and open donor nephrectomy (ODN). MATERIALS AND METHODS: Between January 1997 and January 2008, 241 live donor nephrectomies were performed by either HALDN (n=118) or ODN (n=123). Preoperative patient characteristics were not significantly different between the donors and recipients. We monitored the changes in serum creatinine levels of the donors and recipients preoperatively and on postoperative days 1, 5, 28, 84, and 365. RESULTS: The mean operative times of HALDN and ODN were 171 and 163 minutes (p=0.284), and the mean warm ischemic times were 292 and 236 seconds (p=0.207), respectively. The mean serum creatinine level in the recipients on postoperative day 1 was significantly higher after HALDN than after ODN (3.48 vs. 2.62 mg/dl, p=0.003). However, from postoperative day 5 to 1 year, there was no significant difference between the two groups. The mean serum creatinine level in the donors was not significantly different between the HALDN and ODN groups throughout the study period. CONCLUSIONS: Renal function recovery in the donors was similar with both HALDN and ODN. Graft renal function recovery after HALDN was comparable with that after ODN, except immediately after surgery (postoperative day 1).
Keyword
MeSH Terms
Figure
Reference
-
1. Giessing M. Laparoscopic living-donor nephrectomy. Nephrol Dial Transplant. 2004. 19:Suppl 4. 36–40.2. Ratner LE, Ciseck LJ, Moore RG, Cigarroa FG, Kaufman HS, Kavoussi LR. Laparoscopic live donor nephrectomy. Transplantation. 1995. 60:1047–1049.3. Ratner LE, Kavoussi LR, Schulam PG, Bender JS, Magnuson TH, Montgomery R. Comparison of laparoscopic live donor nephrectomy versus the standard open approach. Transplant Proc. 1997. 29:138–139.4. Yoo KY, Hong SH, Hwang TK. Donor nephrectomy: comparison of open, hand-assisted and laparoscopic donor nephrectomy. Korean J Urol. 2006. 47:1309–1314.5. Sasaki TM, Finelli F, Bugarin E, Fowlkes D, Trollinger J, Barhyte DY, et al. Is laparoscopic donor nephrectomy the new criterion standard? Arch Surg. 2000. 135:943–947.6. Lennerling A, Blohme I, Ostraat O, Lönroth H, Olausson M, Nyberg G. Laparoscopic or open surgery for living donor nephrectomy. Nephrol Dial Transplant. 2001. 16:383–386.7. Vats HS, Rayhill SC, Thomas CP. Early postnephrectomy donor renal function: laparoscopic versus open procedure. Transplantation. 2005. 79:609–612.8. Rawlins MC, Hefty TL, Brown SL, Biehl TR. Learning laparoscopic donor nephrectomy safely: a report on 100 cases. Arch Surg. 2002. 137:531–534.9. Slakey DP, Hahn JC, Rogers E, Rice JC, Gauthier PM, Ruiz-Deya G. Single-center analysis of living donor nephrectomy: hand-assisted laparoscopic, pure laparoscopic, and traditional open. Prog Transplant. 2002. 12:206–211.10. Waller JR, Hiley AL, Mullin EJ, Veitch PS, Nicholson ML. Living kidney donation: a comparison of laparoscopic and conventional open operations. Postgrad Med J. 2002. 78:153–157.11. Branco AW, Kondo W, Branco Filho AJ, George MA, Rangel M, Stunitz LC. A comparison of hand-assisted and pure laparoscopic techniques in live donor nephrectomy. Clinics. 2008. 63:795–800.12. Percegona LS, Bignelli AT, Adamy A Jr, Pilz F, Chin EW, Meyer F, et al. Hand-assisted laparoscopic donor nephrectomy: comparison to pure laparoscopic donor nephrectomy. Transplant Proc. 2008. 40:687–688.13. Nogueira JM, Cangro CB, Fink JC, Schweitzer E, Wiland A, Klassen DK, et al. A comparison of recipient renal outcomes with laparoscopic versus open live donor nephrectomy. Transplantation. 1999. 67:722–728.14. Ratner LE, Montgomery RA, Maley WR, Cohen C, Burdick J, Chavin KD, et al. Laparoscopic live donor nephrectomy: the recipient. Transplantation. 2000. 69:2319–2323.15. Philosophe B, Kuo PC, Schweitzer EJ, Farney AC, Lim JW, Johnson LB, et al. Laparoscopic versus open donor nephrectomy: comparing ureteral complications in the recipients and improving the laparoscopic technique. Transplantation. 1999. 68:497–502.16. Wolf JS Jr, Merion RM, Leichtman AB, Campbell DA Jr, Magee JC, Punch JD, et al. Randomized controlled trial of hand-assisted laparoscopic versus open surgical live donor nephrectomy. Transplantation. 2001. 72:284–290.17. Wolf JS Jr, Tchetgen MB, Merion RM. Hand-assisted laparoscopic live donor nephrectomy. Urology. 1998. 52:885–887.18. Gershbein AB, Fuchs GJ. Hand-assisted and conventional laparoscopic live donor nephrectomy: a comparison of two contemporary techniques. J Endourol. 2002. 16:509–513.19. Kokkinos C, Nanidis T, Antcliffe D, Darzi AW, Tekkis P, Papalois V. Comparison of laparoscopic versus hand-assisted live donor nephrectomy. Transplantation. 2007. 83:41–47.20. Baik S, Rho J, Kim CS. Comparison of hand-assisted laparoscopic donor nephrectomy with open donor nephrectomy. Korean J Urol. 2005. 46:1125–1129.21. London ET, Ho HS, Neuhaus AM, Wolfe BM, Rudich SM, Perez RV. Effect of intravascular volume expansion on renal function during prolonged CO2 pneumoperitoneum. Ann Surg. 2000. 231:195–201.22. Lee BR, Cadeddu JA, Molnar-Nadasdy G, Enriquez D, Nadasdy T, Kavoussi LR, et al. Chronic effect of pneumoperitoneum on renal histology. J Endourol. 1999. 13:279–282.23. Hazebroek EJ, de Bruin RW, Bouvy ND, Marquet RL, Bonthuis F, Bajema IM, et al. Long-term impact of pneumoperitoneum used for laparoscopic donor nephrectomy on renal function and histomorphology in donor and recipient rats. Ann Surg. 2003. 237:351–357.24. McDougall EM, Monk TG, Wolf JS Jr, Hicks M, Clayman RV, Gardner S, et al. The effect of prolonged pneumoperitoneum on renal function in an animal model. J Am Coll Surg. 1996. 182:317–328.25. Kirsch AJ, Hensle TW, Chang DT, Kayton ML, Olsson CA, Sawczuk IS. Renal effects of CO2 insufflation: oliguria and acute renal dysfunction in a rat pneumoperitoneum model. Urology. 1994. 43:453–459.26. Goldfarb DA, Matin SF, Braun WE, Schreiber MJ, Mastroianni B, Papajcik D, et al. Renal outcome 25 years after donor nephrectomy. J Urol. 2001. 166:2043–2047.27. Dols LF, Kok NF, Terkivatan T, Tran KT, Alwayn IP, Weimar W, et al. Optimizing left-sided live kidney donation: hand-assisted retroperitoneoscopic as alternative to standard laparoscopic donor nephrectomy. Transpl Int. 2009. Epub ahead of print.28. Troppmann C, Ormond DB, Perez RV. Laparoscopic (vs open) live donor nephrectomy: a UNOS database analysis of early graft function and survival. Am J Transplant. 2003. 3:1295–1301.29. Jablonski P, Howden BO, Rae DA, Birrell CS, Marshall VC, Tange J. An experimental model for assessment of renal recovery from warm ischemia. Transplantation. 1983. 35:198–204.30. Jacobs SC, Cho E, Dunkin BJ, Flowers JL, Schweitzer E, Cangro C, et al. Laparoscopic live donor nephrectomy: the University of Maryland 3-year experience. J Urol. 2000. 164:1494–1499.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hand-assisted Laparoscopic Live Donor Nephrectomy; Comparison to Open Donor Nephrectomy
- Hand-Assisted Laparoscopic Live Donor Nephrectomy
- Donor Nephrectomy : Comparison of Open, Hand-assisted and Laparoscopic Donor Nephrectomy
- Comparison of Hand-assisted Laparoscopic Donor Nephrectomy with Open Donor Nephrectomy
- Video Assisted Minilaparotomy Surgery (VAMS) - Live Donor Nephrectomy: 239 Cases