Korean J Urol.
2010 Oct;51(10):709-712.
Suprapubic Cystostomy: Risk Analysis of Possible Bowel Interposition Through the Percutaneous Tract by Computed Tomography
- Affiliations
-
- 1Department of Urology, Soonchunhyang University College of Medicine, Seoul, Korea. wonjya@schmc.ac.kr
Abstract
- PURPOSE
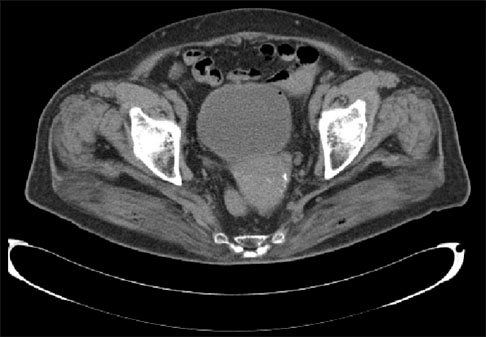
The most serious complication of suprapubic cystostomy is bowel injury. By computed tomography (CT), we investigated the risk factors of possible bowel interposition through the percutaneous suprapubic cystostomy tract.
MATERIALS AND METHODS
From September to October 2009, we consecutively reviewed 795 abdominopelvic CT scans of adult patients performed for various reasons in our hospital. From these scans, we selected the films wherein the urinary bladder was distended more than 6 cm above the symphysis pubis. We then determined whether the bowel was interposed between the bladder and the skin at the routine puncture site of suprapubic cystostomy (the midline of the abdomen 3 cm above the upper margin of the symphysis pubis). We analyzed which factors influenced the possibility of the bowel being interposed between the bladder and the skin at the suprapubic puncture site.
RESULTS
A total of 226 CT (148 males, 78 females) scans were selected. The mean patient age was 63 years (range, 26-84 years). The mean distance between the upper margin of the symphysis pubis and the umbilicus was 14.4 cm (range, 7.2-21.0 cm). In the multivariate analysis, obesity, a positive history of radical pelvic surgery, and a short distance (< or =11 cm) between the symphysis pubis and the umbilicus had significant correlations with bowel interposition in the assumed tract.
CONCLUSIONS
When performing a suprapubic cystostomy, extreme caution is needed to avoid possible bowel injury in patients who are obese, had a previous radical pelvic operation, or have a short distance between the upper margin of the symphysis pubis and the umbilicus.
Keyword
MeSH Terms
Figure
Reference
-
1. Dogra PN, Goel R. Complication of percutaneous suprapubic cystostomy. Int Urol Nephrol. 2004. 36:343–344.2. Flock WD, Litvak AS, McRoberts JW. Evaluation of closed suprapubic cystostomy. Urology. 1978. 11:40–42.3. Hebert DB, Mitchell GW Jr. Perforation of the ileum as a complication of suprapubic catheterization. Obstet Gynecol. 1983. 62:662–664.4. Moody TE, Howards SS, Schneider JA, Rudolf LE. Intestinal obstruction: a complication of percutaneous cystostomy. A case report. J Urol. 1977. 118:680.5. Browning DJ. Potential hazard of suprapubic catheterization. Med J Aust. 1977. 2:580.6. Drutz HP, Khosid HI. Complications with Bonanno suprapubic catheters. Am J Obstet Gynecol. 1984. 149:685–686.7. Simpson RR. An unusual cause of small bowel obstruction: the misplaced suprapubic catheter. J Urol. 2001. 165:1998.8. Lin AC, Wu CC, Wang TL, Chang H. An unusual cause of volvulus: the misplaced suprapubic catheter. J Emerg Med. 2005. 28:219–220.9. Liau SS, Shabeer UA. Laparoscopic management of cecal injury from a misplaced percutaneous suprapubic cystostomy. Surg Laparosc Endosc Percutan Tech. 2005. 15:378–379.10. Ballentine HC, David YC. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Basic instrumentation and cystoscopy. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;161–170.11. Engel WJ. Suprapubic trocar cystostomy: an evaluation and presentation of an improved instrument. J Urol. 1951. 65:998–1005.12. Alagiri M, Seidmon EJ. Percutaneous endoscopic cystostomy for bladder localization and exact placement of a suprapubic tube. J Urol. 1998. 159:963–964.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of the Preliminary Ultrasonographic Examination before Suprapubic Cystostomy by Trocar
- Squamous Cell Carcinoma of the Suprapubic Cystostomy Tract With Bladder Involvement
- A Comprehensive Review of Percutaneous Nephrostomy and Suprapubic Cystostomy
- Intraurethral Instillation of 5-fluorouracil with Suprapubic Cystostomy for Intraurethral Condyloma Acuminatum
- Clinicel Observetion of Urethroplasty after Suprapubic Cystostomy in 11 Cases Urethral Injuries