Obstet Gynecol Sci.
2015 Mar;58(2):90-97. 10.5468/ogs.2015.58.2.90.
Clinical characteristics and perinatal outcome of fetal hydrops
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. drmaxmix.choi@samsung.com
- KMID: 2314031
- DOI: http://doi.org/10.5468/ogs.2015.58.2.90
Abstract
OBJECTIVE
To investigate the clinical characteristics of fetal hydrops and to find the antenatal ultrasound findings predictive of adverse perinatal outcome.
METHODS
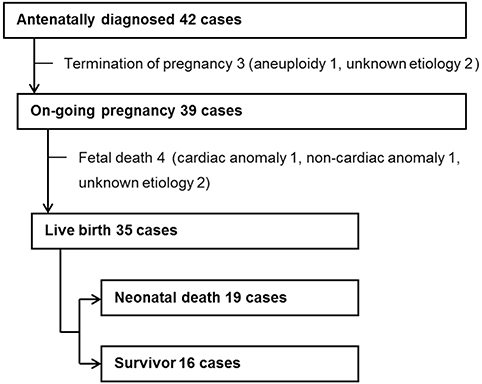
This is a retrospective study of 42 women with fetal hydrops who delivered in a tertiary-referral center from 2005 to 2013. Fetal hydrops was defined as the presence of fluid collection in > or =2 body cavities: ascites, pleural effusion, pericardial effusion, and skin edema. Predictor variables recorded included: maternal characteristics, gestational age at diagnosis, ultrasound findings, and identifiable causes. Primary outcome variables analyzed were fetal death and neonatal death.
RESULTS
The mean gestational age at diagnosis was 29.3+/-5.4 weeks (range, 18 to 39 weeks). The most common identifiable causes were cardiac abnormality (10), followed by syndrome (4), aneuploidy (3), congenital infection (3), twin-to-twin transfusion syndrome (3), non-cardiac anormaly (2), chorioangioma (2), inborn errors of metabolism (1), and immune hydrops by anti-E antibody isoimmunization (1). Thirteen cases had no definite identifiable causes. Three women elected termination of pregnancy. Fetal death occurred in 4 cases. Among the 35 live-born babies, only 16 survived (54.0% neonatal mortality rate). Fetal death and neonatal mortality rate was not significantly associated with Doppler velocimetry indices or location of fluid collection, but increasing numbers of fluid collection site was significantly associated with a higher risk of neonatal death.
CONCLUSION
The incidence of fetal hydrops in our retrospective study was 24.4 per 10,000 deliveries and the perinatal mortality rate was 61.9% (26/42). The number of fluid collection sites was the significant antenatal risk factor to predict neonatal death.
MeSH Terms
Figure
Cited by 1 articles
-
Infant, maternal, and perinatal mortality statistics in the Republic of Korea, 2014
, Hyun-Young Shin, Ji-Youn Lee, Juhwa Song, Seokmin Lee, Junghun Lee, Byeongsun Lim, Heyran Kim, Sun Huh
J Korean Med Assoc. 2017;60(7):588-597. doi: 10.5124/jkma.2017.60.7.588.
Reference
-
1. Bellini C, Hennekam RC. Non-immune hydrops fetalis: a short review of etiology and pathophysiology. Am J Med Genet A. 2012; 158A:597–605.2. Randenberg AL. Nonimmune hydrops fetalis part I: etiology and pathophysiology. Neonatal Netw. 2010; 29:281–295.3. Favre R, Dreux S, Dommergues M, Dumez Y, Luton D, Oury JF, et al. Nonimmune fetal ascites: a series of 79 cases. Am J Obstet Gynecol. 2004; 190:407–412.4. Randenberg AL. Nonimmune hydrops fetalis part II: does etiology influence mortality? Neonatal Netw. 2010; 29:367–380.5. Abrams ME, Meredith KS, Kinnard P, Clark RH. Hydrops fetalis: a retrospective review of cases reported to a large national database and identification of risk factors associated with death. Pediatrics. 2007; 120:84–89.6. Liao C, Wei J, Li Q, Li J, Li L, Li D. Nonimmune hydrops fetalis diagnosed during the second half of pregnancy in Southern China. Fetal Diagn Ther. 2007; 22:302–305.7. Heinonen S, Ryynanen M, Kirkinen P. Etiology and outcome of second trimester non-immunologic fetal hydrops. Acta Obstet Gynecol Scand. 2000; 79:15–18.8. Hutchison AA, Drew JH, Yu VY, Williams ML, Fortune DW, Beischer NA. Nonimmunologic hydrops fetalis: a review of 61 cases. Obstet Gynecol. 1982; 59:347–352.9. Simpson JH, McDevitt H, Young D, Cameron AD. Severity of non-immune hydrops fetalis at birth continues to predict survival despite advances in perinatal care. Fetal Diagn Ther. 2006; 21:380–382.10. Moreno CA, Kanazawa T, Barini R, Nomura ML, Andrade KC, Gomes CP, et al. Non-immune hydrops fetalis: a prospective study of 53 cases. Am J Med Genet A. 2013; 161A:3078–3086.11. Fukushima K, Morokuma S, Fujita Y, Tsukimori K, Satoh S, Ochiai M, et al. Short-term and long-term outcomes of 214 cases of non-immune hydrops fetalis. Early Hum Dev. 2011; 87:571–575.12. Sohan K, Carroll SG, De La Fuente S, Soothill P, Kyle P. Analysis of outcome in hydrops fetalis in relation to gestational age at diagnosis, cause and treatment. Acta Obstet Gynecol Scand. 2001; 80:726–730.13. Nakayama H, Kukita J, Hikino S, Nakano H, Hara T. Long-term outcome of 51 liveborn neonates with nonimmune hydrops fetalis. Acta Paediatr. 1999; 88:24–28.14. Bellini C, Hennekam RC, Fulcheri E, Rutigliani M, Morcaldi G, Boccardo F, et al. Etiology of nonimmune hydrops fetalis: a systematic review. Am J Med Genet A. 2009; 149A:844–851.15. Baschat AA. Arterial and venous Doppler in the diagnosis and management of early onset fetal growth restriction. Early Hum Dev. 2005; 81:877–887.16. Bilardo CM, Wolf H, Stigter RH, Ville Y, Baez E, Visser GH, et al. Relationship between monitoring parameters and perinatal outcome in severe, early intrauterine growth restriction. Ultrasound Obstet Gynecol. 2004; 23:119–125.17. Hofstaetter C, Hansmann M, Eik-Nes SH, Huhta JC, Luther SL. A cardiovascular profile score in the surveillance of fetal hydrops. J Matern Fetal Neonatal Med. 2006; 19:407–413.18. Mari G, Deter RL, Carpenter RL, Rahman F, Zimmerman R, Moise KJ Jr, et al. Noninvasive diagnosis by Doppler ultrasonography of fetal anemia due to maternal red-cell alloimmunization. Collaborative Group for Doppler Assessment of the Blood Velocity in Anemic Fetuses. N Engl J Med. 2000; 342:9–14.19. Berg C, Kremer C, Geipel A, Kohl T, Germer U, Gembruch U. Ductus venosus blood flow alterations in fetuses with obstructive lesions of the right heart. Ultrasound Obstet Gynecol. 2006; 28:137–142.20. Smoleniec J, James D. Predictive value of pleural effusions in fetal hydrops. Fetal Diagn Ther. 1995; 10:95–100.21. Kim SA, Lee SM, Hong JS, Lee J, Park CW, Kim BJ, et al. Ultrasonographic severity scoring of non-immune hydrops: a predictor of perinatal mortality. J Perinat Med. 2014; 05. 15. 10:95–100. [Epub]. DOI: 10.1515/jpm-2013-0208.22. Suwanrath-Kengpol C, Kor-anantakul O, Suntharasaj T, Leetanaporn R. Etiology and outcome of non-immune hydrops fetalis in southern Thailand. Gynecol Obstet Invest. 2005; 59:134–137.23. Mostello DJ, Bofinger MK, Siddiqi TA. Spontaneous resolution of fetal cystic hygroma and hydrops in Turner syndrome. Obstet Gynecol. 1989; 73:862–865.24. Swain S, Cameron AD, McNay MB, Howatson AG. Prenatal diagnosis and management of nonimmune hydrops fetalis. Aust N Z J Obstet Gynaecol. 1999; 39:285–290.25. Petrikovsky BM, Baker D, Schneider E. Fetal hydrops secondary to human parvovirus infection in early pregnancy. Prenat Diagn. 1996; 16:342–344.26. Henrich W, Heeger J, Schmider A, Dudenhausen JW. Complete spontaneous resolution of severe nonimmunological hydrops fetalis with unknown etiology in the second trimester: a case report. J Perinat Med. 2002; 30:522–527.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of fetal atrial flutter with hydrops fetalis
- Clinical Diversities and Perinatal Outcomes of Nonimmune Hydrops Fetalis
- An unusual prenatal manifestation of a huge congenital cystic adenomatoid malformation with favorable perinatal outcome
- A Case of Placental Chorioangioma Combined with Non-immune Hydrops Fetalis
- Fetal pulmonary sequestration complicated hydrops: Successful fetal therapy by thoracoamniotic shunting