Nutr Res Pract.
2015 Apr;9(2):180-185. 10.4162/nrp.2015.9.2.180.
Effect of sodium restriction on blood pressure of unstable or uncontrolled hypertensive patients in primary care
- Affiliations
-
- 1Department of Bio- and food sciences, University College Ghent, B-9000 Ghent, Belgium. willem.dekeyzer@hogent.be
- 2Faculty of Medicine and Health Sciences, Ghent University, B-9000 Ghent, Belgium.
- 3General practice Vossensteert Sint-Jozef, B-8000 Bruges, Belgium.
- 4Department of Public Health, Faculty of Medicine and Health Sciences, Ghent University, B-9000 Ghent, Belgium.
- KMID: 2313827
- DOI: http://doi.org/10.4162/nrp.2015.9.2.180
Abstract
- BACKGROUND/OBJECTIVES
The aims of the present study are: 1) to quantify sodium consumption of patients with unstable or uncontrolled hypertension, 2) to investigate if reduced sodium intake can lower BP in these patients, and 3), to assess the acceptability and feasibility of this approach.
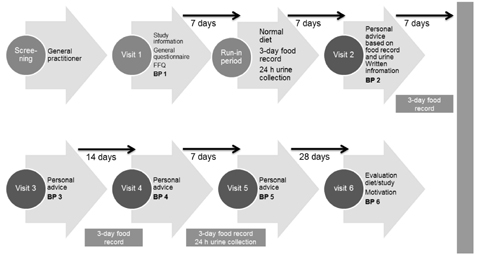
SUBJECTS/METHODS
This study included 25 adults (age: 50+ years) with frequently elevated BP or patients with uncontrolled, uncomplicated hypertension despite drug treatment in a general practice setting. BP and salt intake (24h urinary excretion and food records) were measured at baseline and after a sodium reduced diet.
RESULTS
Mean (+/- SD) systolic (SBP) over diastolic (DBP) blood pressure (mmHg) at baseline was 150.7 (+/- 9.5)/84.149 (+/- 5.6). Mean urinary sodium excretion was 146 mmol/24h. A reduction of 28 mmol sodium excretion decreased SBP/DBP to 135.5 (+/- 13.0)/82.5 (+/- 12.8) (P < 0.001). After one month of no dietary advice, only in 48%, SBP was still < or =140 mmHg.
CONCLUSION
Assessment of sodium intake using food records, 24h urine collections and probing questions to identify use of sodium containing supplements or drugs are essential for tailored advice targeted at sodium intake reduction. The results of the present study indicate that reduced sodium intake can lower BP after 4 weeks in unstable or uncontrolled hypertensive patients.
Keyword
MeSH Terms
Figure
Reference
-
1. He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009; 23:363–384.
Article2. Lawes CM, Vander Hoorn S, Rodgers A. International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008; 371:1513–1518.
Article3. Mohan S, Campbell NR. Salt and high blood pressure. Clin Sci (Lond). 2009; 117:1–11.
Article4. Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR. Writing Group of the PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003; 289:2083–2093.5. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ. National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42:1206–1252.
Article6. He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002; 16:761–770.
Article7. Krauss RM, Eckel RH, Howard B, Appel LJ, Daniels SR, Deckelbaum RJ, Erdman JW Jr, Kris-Etherton P, Goldberg IJ, Kotchen TA, Lichtenstein AH, Mitch WE, Mullis R, Robinson K, Wylie-Rosett J, St Jeor S, Suttie J, Tribble DL, Bazzarre TL. AHA Dietary Guidelines: revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation. 2000; 102:2284–2299.8. Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. American Heart Association. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006; 47:296–308.
Article9. He FJ, MacGregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev. 2004; CD004937.
Article10. World Health Organization Regional Office for Europe (DK). Estimation of Sodium Intake and Output: Review of Methods and Recommendations for Epidemiological Studies: Report on a WHO Meeting by the WHO Collaborating Center for Research and Training in Cardiovascular Diseases. Geneva: World Health Organization;1984.11. Huybrechts I, Geelen A, de Vries JH, Casagrande C, Nicolas G, De Keyzer W, Lillegaard IT, Ruprich J, Lafay L, Wilson-van den Hooven EC, Niekerk EM, Margaritis I, Rehurkova I, Crispim SP, Freisling H, De Henauw S, Slimani N. EFCOVAL Consortium. Respondents' evaluation of the 24-h dietary recall method (EPIC-Soft) in the EFCOVAL Project. Eur J Clin Nutr. 2011; 65:Suppl 1. S29–S37.
Article12. Franco V, Oparil S. Salt sensitivity, a determinant of blood pressure, cardiovascular disease and survival. J Am Coll Nutr. 2006; 25:247S–255S.
Article13. MacGregor GA, Markandu ND, Sagnella GA, Singer DR, Cappuccio FP. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension. Lancet. 1989; 2:1244–1247.
Article14. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, Karanja N, Lin PH. DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001; 344:3–10.
Article15. Karanja NM, Obarzanek E, Lin PH, McCullough ML, Phillips KM, Swain JF, Champagne CM, Hoben KP. Descriptive characteristics of the dietary patterns used in the Dietary Approaches to Stop Hypertension Trial. DASH Collaborative Research Group. J Am Diet Assoc. 1999; 99:S19–S27.16. Miller ER 3rd, Erlinger TP, Young DR, Jehn M, Charleston J, Rhodes D, Wasan SK, Appel LJ. Results of the Diet, Exercise, and Weight Loss Intervention Trial (DEW-IT). Hypertension. 2002; 40:612–618.
Article17. Miller ER Jr, Erlinger TP, Young DR, Prokopowicz GP, Appel LJ. Lifestyle changes that reduce blood pressure: implementation in clinical practice. J Clin Hypertens (Greenwich). 1999; 1:191–198.18. Wang CY, Cogswell ME, Loria CM, Chen TC, Pfeiffer CM, Swanson CA, Caldwell KL, Perrine CG, Carriquiry AL, Liu K, Sempos CT, Gillespie CD, Burt VL. Urinary excretion of sodium, potassium, and chloride, but not iodine, varies by timing of collection in a 24-hour calibration study. J Nutr. 2013; 143:1276–1282.
Article19. Cogswell ME, Wang CY, Chen TC, Pfeiffer CM, Elliott P, Gillespie CD, Carriquiry AL, Sempos CT, Liu K, Perrine CG, Swanson CA, Caldwell KL, Loria CM. Validity of predictive equations for 24-h urinary sodium excretion in adults aged 18-39 y. Am J Clin Nutr. 2013; 98:1502–1513.
Article20. Douglas L, Akil M. Sodium in soluble paracetamol may be linked to raised blood pressure. BMJ. 2006; 332:1133.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Comparison of Renal Handling of Sodium and Potassium According to Salt Intake between Control and Hypertensive Group
- Salt, Hypertension, and Cardiovascular Diseases
- Dietary Salt and Potassium Intake and Hypertension
- The Effect of Sodium Nitroprusside on Responsed of the Cardiovascular System during Endotracheal intubation
- Clinical Observation on the Effect of Parenteral Reserpine