Nutr Res Pract.
2015 Apr;9(2):165-173. 10.4162/nrp.2015.9.2.165.
No short-term effects of calorie-controlled Mediterranean or fast food dietary interventions on established biomarkers of vascular or metabolic risk in healthy individuals
- Affiliations
-
- 1Department of Internal Medicine I and Clinical Chemistry, University of Heidelberg, Im Neuenheimer Feld 410, 69120 Heidelberg, Germany. maik.brune@med.uni-heidelberg.de
- 2Division of Molecular Metabolic Control, German Cancer Research Center (DKFZ) Heidelberg, Im Neuenheimer Feld 280, 69120 Heidelberg, Germany.
- 3Department of Cellular Immunology, Institute of Immunology, Rockefellerova 2, 10000 Zagreb, Croatia.
- KMID: 2313825
- DOI: http://doi.org/10.4162/nrp.2015.9.2.165
Abstract
- BACKGROUND/OBJECTIVES
This study addressed the question whether the composition of supposedly 'healthy' or 'unhealthy' dietary regimes has a calorie-independent short-term effect on biomarkers of metabolic stress and vascular risk in healthy individuals.
SUBJECTS/METHODS
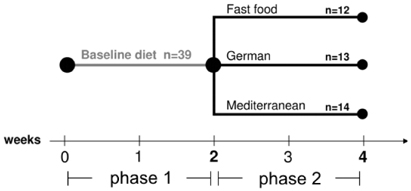
Healthy male volunteers (age 29.5 +/- 5.9 years, n = 39) were given a standardized baseline diet for two weeks before randomization into three groups of different dietary regimes: fast food, Mediterranean and German cooking style. Importantly, the amount of calories consumed per day was identical in all three groups. Blood samples were analyzed for biomarkers of cardiovascular risk and metabolic stress after two weeks of the baseline diet and after two weeks of the assigned dietary regime.
RESULTS
No dietary intervention affected the metabolic or cardiovascular risk profile when compared in-between groups or compared to baseline. Subjects applied to the Mediterranean diet showed a statistically significant increase of uric acid compared to baseline and compared to the German diet group. Plasma concentrations of urea were significantly higher in both the fast food group and the Mediterranean group, when compared to baseline and compared to the German diet group. No significant differences were detected for the levels of vitamins, trace elements or metabolic stress markers (8-hydroxy-2-deoxyguanosine, malondialdehyde and methylglyoxal, a potent glycating agent). Established parameters of vascular risk (e.g. LDL-cholesterol, lipoprotein(a), homocysteine) were not significantly changed in-between groups or compared to baseline during the intervention period.
CONCLUSIONS
The calorie-controlled dietary intervention caused neither protective nor harmful short-term effects regarding established biomarkers of vascular or metabolic risk. When avoiding the noxious effects of overfeeding, healthy individuals can possess the metabolic capacity to compensate for a potentially disadvantageous composition of a certain diet.
MeSH Terms
Figure
Reference
-
1. Prentice AM, Jebb SA. Fast foods, energy density and obesity: a possible mechanistic link. Obes Rev. 2003; 4:187–194.
Article2. Urpi-Sarda M, Casas R, Chiva-Blanch G, Romero-Mamani ES, Valderas-Martínez P, Salas-Salvadó J, Covas MI, Toledo E, Andres-Lacueva C, Llorach R, García-Arellano A, Bulló M, Ruiz-Gutierrez V, Lamuela-Raventos RM, Estruch R. The Mediterranean diet pattern and its main components are associated with lower plasma concentrations of tumor necrosis factor receptor 60 in patients at high risk for cardiovascular disease. J Nutr. 2012; 142:1019–1025.
Article3. Bédard A, Riverin M, Dodin S, Corneau L, Lemieux S. Sex differences in the impact of the Mediterranean diet on cardiovascular risk profile. Br J Nutr. 2012; 108:1428–1434.
Article4. de Lorgeril M, Salen P. Mediterranean diet in secondary prevention of CHD. Public Health Nutr. 2011; 14:2333–2337.
Article5. Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010; 92:1189–1196.
Article6. Sofi F, Macchi C, Abbate R, Gensini GF, Casini A. Effectiveness of the Mediterranean diet: can it help delay or prevent Alzheimer's disease? J Alzheimers Dis. 2010; 20:795–801.
Article7. Giacosa A, Barale R, Bavaresco L, Gatenby P, Gerbi V, Janssens J, Johnston B, Kas K, La Vecchia C, Mainguet P, Morazzoni P, Negri E, Pelucchi C, Pezzotti M, Rondanelli M. Cancer prevention in Europe: the Mediterranean diet as a protective choice. Eur J Cancer Prev. 2013; 22:90–95.8. Ben-Avraham S, Harman-Boehm I, Schwarzfuchs D, Shai I. Dietary strategies for patients with type 2 diabetes in the era of multi-approaches; review and results from the Dietary Intervention Randomized Controlled Trial (DIRECT). Diabetes Res Clin Pract. 2009; 86:Suppl 1. S41–S48.
Article9. Pérez-Martínez P, García-Ríos A, Delgado-Lista J, Pérez-Jiménez F, López-Miranda J. Mediterranean diet rich in olive oil and obesity, metabolic syndrome and diabetes mellitus. Curr Pharm Des. 2011; 17:769–777.
Article10. Vincent-Baudry S, Defoort C, Gerber M, Bernard MC, Verger P, Helal O, Portugal H, Planells R, Grolier P, Amiot-Carlin MJ, Vague P, Lairon D. The Medi-RIVAGE study: reduction of cardiovascular disease risk factors after a 3-mo intervention with a Mediterranean-type diet or a low-fat diet. Am J Clin Nutr. 2005; 82:964–971.
Article11. Martínez-González MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z, Benito S, Tortosa A, Bes-Rastrollo M. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ. 2008; 336:1348–1351.
Article12. Morrison AC, Ness RB. Sodium intake and cardiovascular disease. Annu Rev Public Health. 2011; 32:71–90.
Article13. Wexler R, Pleister A, Raman SV, Borchers JR. Therapeutic lifestyle changes for cardiovascular disease. Phys Sportsmed. 2012; 40:109–115.
Article14. Wheeler ML, Dunbar SA, Jaacks LM, Karmally W, Mayer-Davis EJ, Wylie-Rosett J, Yancy WS Jr. Macronutrients, food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care. 2012; 35:434–445.
Article15. Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Martínez-González MA. PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013; 368:1279–1290.
Article16. Hoermann R, Grossmann M. Mediterranean diet for primary prevention of cardiovascular disease. N Engl J Med. 2013; 369:674.
Article17. Kopel E, Sidi Y, Kivity S. Mediterranean diet for primary prevention of cardiovascular disease. N Engl J Med. 2013; 369:672.
Article18. Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR Jr, Ludwig DS. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005; 365:36–42.
Article19. Krebs JD, Elley CR, Parry-Strong A, Lunt H, Drury PL, Bell DA, Robinson E, Moyes SA, Mann JI. The Diabetes Excess Weight Loss (DEWL) Trial: a randomised controlled trial of high-protein versus high-carbohydrate diets over 2 years in type 2 diabetes. Diabetologia. 2012; 55:905–914.
Article20. TODAY Study Group. Zeitler P, Hirst K, Pyle L, Linder B, Copeland K, Arslanian S, Cuttler L, Nathan DM, Tollefsen S, Wilfley D, Kaufman F. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med. 2012; 366:2247–2256.
Article21. Black RN, Spence M, McMahon RO, Cuskelly GJ, Ennis CN, McCance DR, Young IS, Bell PM, Hunter SJ. Effect of eucaloric high- and low-sucrose diets with identical macronutrient profile on insulin resistance and vascular risk: a randomized controlled trial. Diabetes. 2006; 55:3566–3572.
Article22. Akesson A, Andersen LF, Kristjánsdóttir AG, Roos E, Trolle E, Voutilainen E, Wirfält E. Health effects associated with foods characteristic of the Nordic diet: a systematic literature review. Food Nutr Res. 2013; 57.23. Lindeberg S, Jönsson T, Granfeldt Y, Borgstrand E, Soffman J, Sjöström K, Ahrén B. A Palaeolithic diet improves glucose tolerance more than a Mediterranean-like diet in individuals with ischaemic heart disease. Diabetologia. 2007; 50:1795–1807.
Article24. Ambring A, Friberg P, Axelsen M, Laffrenzen M, Taskinen MR, Basu S, Johansson M. Effects of a Mediterranean-inspired diet on blood lipids, vascular function and oxidative stress in healthy subjects. Clin Sci (Lond). 2004; 106:519–525.
Article25. Athyros VG, Kakafika AI, Papageorgiou AA, Tziomalos K, Peletidou A, Vosikis C, Karagiannis A, Mikhailidis DP. Effect of a plant stanol ester-containing spread, placebo spread, or Mediterranean diet on estimated cardiovascular risk and lipid, inflammatory and haemostatic factors. Nutr Metab Cardiovasc Dis. 2011; 21:213–221.
Article26. Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, Fiol M, Gómez-Gracia E, López-Sabater MC, Vinyoles E, Arós F, Conde M, Lahoz C, Lapetra J, Sáez G, Ros E. PREDIMED Study Investigators. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006; 145:1–11.27. Rees K, Hartley L, Flowers N, Clarke A, Hooper L, Thorogood M, Stranges S. 'Mediterranean' dietary pattern for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013; 8:CD009825.
Article28. Fitó M, Guxens M, Corella D, Sáez G, Estruch R, de la Torre R, Francés F, Cabezas C, López-Sabater Mdel C, Marrugat J, García-Arellano A, Arós F, Ruiz-Gutierrez V, Ros E, Salas-Salvadó J, Fiol M, Solá R, Covas MI. PREDIMED Study Investigators. Effect of a traditional Mediterranean diet on lipoprotein oxidation: a randomized controlled trial. Arch Intern Med. 2007; 167:1195–1203.
Article29. Kim JY, Yang YJ, Yang YK, Oh SY, Hong YC, Lee EK, Kwon O. Diet quality scores and oxidative stress in Korean adults. Eur J Clin Nutr. 2011; 65:1271–1278.
Article30. Urquiaga I, Strobel P, Perez D, Martinez C, Cuevas A, Castillo O, Marshall G, Rozowski J, Leighton F. Mediterranean diet and red wine protect against oxidative damage in young volunteers. Atherosclerosis. 2010; 211:694–699.
Article31. Bierhaus A, Fleming T, Stoyanov S, Leffler A, Babes A, Neacsu C, Sauer SK, Eberhardt M, Schnölzer M, Lasitschka F, Neuhuber WL, Kichko TI, Konrade I, Elvert R, Mier W, Pirags V, Lukic IK, Morcos M, Dehmer T, Rabbani N, Thornalley PJ, Edelstein D, Nau C, Forbes J, Humpert PM, Schwaninger M, Ziegler D, Stern DM, Cooper ME, Haberkorn U, Brownlee M, Reeh PW, Nawroth PP. Methylglyoxal modification of Nav1.8 facilitates nociceptive neuron firing and causes hyperalgesia in diabetic neuropathy. Nat Med. 2012; 18:926–933.
Article32. Keys A, Anderson JT, Grande F. Prediction of serum-cholesterol responses of man to changes in fats in the diet. Lancet. 1957; 273:959–966.
Article33. Layman DK, Boileau RA, Erickson DJ, Painter JE, Shiue H, Sather C, Christou DD. A reduced ratio of dietary carbohydrate to protein improves body composition and blood lipid profiles during weight loss in adult women. J Nutr. 2003; 133:411–417.
Article34. Mensink RP, Katan MB. Effect of monounsaturated fatty acids versus complex carbohydrates on high-density lipoproteins in healthy men and women. Lancet. 1987; 1:122–125.
Article35. Müller H, Jordal O, Kierulf P, Kirkhus B, Pedersen JI. Replacement of partially hydrogenated soybean oil by palm oil in margarine without unfavorable effects on serum lipoproteins. Lipids. 1998; 33:879–887.
Article36. Noakes M, Keogh JB, Foster PR, Clifton PM. Effect of an energy-restricted, high-protein, low-fat diet relative to a conventional high-carbohydrate, low-fat diet on weight loss, body composition, nutritional status, and markers of cardiovascular health in obese women. Am J Clin Nutr. 2005; 81:1298–1306.
Article37. Beisswenger PJ, Howell SK, O'Dell RM, Wood ME, Touchette AD, Szwergold BS. alpha-Dicarbonyls increase in the postprandial period and reflect the degree of hyperglycemia. Diabetes Care. 2001; 24:726–732.
Article38. Gregersen S, Samocha-Bonet D, Heilbronn LK, Campbell LV. Inflammatory and oxidative stress responses to high-carbohydrate and high-fat meals in healthy humans. J Nutr Metab. 2012; 2012:238056.
Article39. Vetrani C, Costabile G, Di Marino L, Rivellese AA. Nutrition and oxidative stress: a systematic review of human studies. Int J Food Sci Nutr. 2013; 64:312–326.
Article40. Deutsche Gesellschaft für Ernährung. Österreichische Gesellschaft für Ernährung. Schweizerische Gesellschaft für Ernährungsforschung. Schweizerische Vereinigung für Ernährung. Referenzwerte für die Nährstoffzufuhr. 1. Auflage: 4. Korrigierter Nachdruck. Neustadt an der Weinstraße: Neuer Umschau Buchverlag;2012.41. Baker EM, Saari JC, Tolbert BM. Ascorbic acid metabolism in man. Am J Clin Nutr. 1966; 19:371–378.
Article42. Carr AC, Frei B. Toward a new recommended dietary allowance for vitamin C based on antioxidant and health effects in humans. Am J Clin Nutr. 1999; 69:1086–1107.
Article43. Ohrvik VE, Witthoft CM. Human folate bioavailability. Nutrients. 2011; 3:475–490.
Article44. Sauberlich HE, Kretsch MJ, Skala JH, Johnson HL, Taylor PC. Folate requirement and metabolism in nonpregnant women. Am J Clin Nutr. 1987; 46:1016–1028.
Article45. Sui H, Wang W, Wang PH, Liu LS. Effect of glutathione peroxidase mimic ebselen (PZ51) on endothelium and vascular structure of stroke-prone spontaneously hypertensive rats. Blood Press. 2005; 14:366–372.
Article46. Richard JP. Mechanism for the formation of methylglyoxal from triosephosphates. Biochem Soc Trans. 1993; 21:549–553.
Article47. Prochaska LJ, Nguyen XT, Donat N, Piekutowski WV. Effects of food processing on the thermodynamic and nutritive value of foods: literature and database survey. Med Hypotheses. 2000; 54:254–262.
Article48. Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008; 9:535–547.
Article49. Desai KM, Chang T, Wang H, Banigesh A, Dhar A, Liu J, Untereiner A, Wu L. Oxidative stress and aging: is methylglyoxal the hidden enemy? Can J Physiol Pharmacol. 2010; 88:273–284.50. Fleming TH, Humpert PM, Nawroth PP, Bierhaus A. Reactive metabolites and AGE/RAGE-mediated cellular dysfunction affect the aging process: a mini-review. Gerontology. 2011; 57:435–443.51. Sarri K, Bertsias G, Linardakis M, Tsibinos G, Tzanakis N, Kafatos A. The effect of periodic vegetarianism on serum retinol and alpha-tocopherol levels. Int J Vitam Nutr Res. 2009; 79:271–280.
Article52. Trepanowski JF, Bloomer RJ. The impact of religious fasting on human health. Nutr J. 2010; 9:57.
Article53. Rudolph TK, Ruempler K, Schwedhelm E, Tan-Andresen J, Riederer U, Böger RH, Maas R. Acute effects of various fast-food meals on vascular function and cardiovascular disease risk markers: the Hamburg Burger Trial. Am J Clin Nutr. 2007; 86:334–340.
Article54. Papadaki A, Scott JA. Follow-up of a web-based tailored intervention promoting the Mediterranean diet in Scotland. Patient Educ Couns. 2008; 73:256–263.
Article55. Hansen AS, Marckmann P, Dragsted LO, Finné Nielsen IL, Nielsen SE, Grønbaek M. Effect of red wine and red grape extract on blood lipids, haemostatic factors, and other risk factors for cardiovascular disease. Eur J Clin Nutr. 2005; 59:449–455.
Article56. Wismann J, Willoughby D. Gender differences in carbohydrate metabolism and carbohydrate loading. J Int Soc Sports Nutr. 2006; 3:28–34.
Article57. Clausen JO, Borch-Johnsen K, Ibsen H, Bergman RN, Hougaard P, Winther K, Pedersen O. Insulin sensitivity index, acute insulin response, and glucose effectiveness in a population-based sample of 380 young healthy Caucasians. Analysis of the impact of gender, body fat, physical fitness, and life-style factors. J Clin Invest. 1996; 98:1195–1209.
Article58. Hollenbeck C, Reaven GM. Variations in insulin-stimulated glucose uptake in healthy individuals with normal glucose tolerance. J Clin Endocrinol Metab. 1987; 64:1169–1173.
Article59. Fielding CJ, Havel RJ, Todd KM, Yeo KE, Schloetter MC, Weinberg V, Frost PH. Effects of dietary cholesterol and fat saturation on plasma lipoproteins in an ethnically diverse population of healthy young men. J Clin Invest. 1995; 95:611–618.
Article60. Johnstone AM, Murison SD, Duncan JS, Rance KA, Speakman JR. Factors influencing variation in basal metabolic rate include fat-free mass, fat mass, age, and circulating thyroxine but not sex, circulating leptin, or triiodothyronine. Am J Clin Nutr. 2005; 82:941–948.
Article61. Norum KR, Blomhoff R. McCollum Award Lecture, 1992: vitamin A absorption, transport, cellular uptake, and storage. Am J Clin Nutr. 1992; 56:735–744.
Article62. Talegawkar SA, Johnson EJ, Carithers T, Taylor HA Jr, Bogle ML, Tucker KL. Total alpha-tocopherol intakes are associated with serum alpha-tocopherol concentrations in African American adults. J Nutr. 2007; 137:2297–2303.
Article63. Levine M, Rumsey SC, Daruwala R, Park JB, Wang Y. Criteria and recommendations for vitamin C intake. JAMA. 1999; 281:1415–1423.
Article64. Hung J, Abratte CM, Wang W, Li R, Moriarty DJ, Caudill MA. Ethnicity and folate influence choline status in young women consuming controlled nutrient intakes. J Am Coll Nutr. 2008; 27:253–259.
Article65. Gregory JF 3rd, Williamson J, Liao JF, Bailey LB, Toth JP. Kinetic model of folate metabolism in nonpregnant women consuming [2H2]folic acid: isotopic labeling of urinary folate and the catabolite para-acetamidobenzoylglutamate indicates slow, intake-dependent, turnover of folate pools. J Nutr. 1998; 128:1896–1906.
Article66. Horwitt MK, Elliott WH, Kanjananggulpan P, Fitch CD. Serum concentrations of alpha-tocopherol after ingestion of various vitamin E preparations. Am J Clin Nutr. 1984; 40:240–245.
Article67. Kallner A, Hartmann D, Hornig D. Steady-state turnover and body pool of ascorbic acid in man. Am J Clin Nutr. 1979; 32:530–539.
Article68. Bierhaus A, Wolf J, Andrassy M, Rohleder N, Humpert PM, Petrov D, Ferstl R, von Eynatten M, Wendt T, Rudofsky G, Joswig M, Morcos M, Schwaninger M, McEwen B, Kirschbaum C, Nawroth PP. A mechanism converting psychosocial stress into mononuclear cell activation. Proc Natl Acad Sci U S A. 2003; 100:1920–1925.
Article69. Held C, Iqbal R, Lear SA, Rosengren A, Islam S, Mathew J, Yusuf S. Physical activity levels, ownership of goods promoting sedentary behaviour and risk of myocardial infarction: results of the INTERHEART study. Eur Heart J. 2012; 33:452–466.
Article70. van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HF, van den Borne BH. Social support in diabetes: a systematic review of controlled intervention studies. Patient Educ Couns. 2005; 59:1–12.
Article71. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, Keinänen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, Uusitupa M. Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001; 344:1343–1350.
Article72. Rees K, Dyakova M, Ward K, Thorogood M, Brunner E. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev. 2013; 3:CD002128.
Article73. Cascio G, Schiera G, Di Liegro I. Dietary fatty acids in metabolic syndrome, diabetes and cardiovascular diseases. Curr Diabetes Rev. 2012; 8:2–17.
Article74. Vessby B, Karlström B, Ohrvall M, Järvi A, Andersson A, Basu S. Diet, nutrition and diabetes mellitus. Ups J Med Sci. 2000; 105:151–160.
Article75. Wilkin TJ. Early nutrition and diabetes mellitus. BMJ. 1993; 306:283–284.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Eating, diet, and nutrition for the treatment of non-alcoholic fatty liver disease
- Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance
- Short-term Effects of Eating Behavior Modification on Metabolic Syndrome-Related Risks in Overweight and Obese Korean Adults
- Relationship between Obesity and Korean and Mediterranean Dietary Patterns: A Review of the Literature
- Effects of a Portfolio-Mediterranean Diet and a Mediterranean Diet with or without a Sterol-Enriched Yogurt in Individuals with Hypercholesterolemia