Lab Med Online.
2014 Apr;4(2):85-90.
Usefulness of Procalcitonin in the Diagnosis of Early Neonatal Bacterial Infection
- Affiliations
-
- 1Department of Laboratory Medicine, College of Medicine, Chungnam National University, Daejeon, Korea. kckwon@cnu.ac.kr
- 2Department of Pediatrics, College of Medicine, Chungnam National University, Daejeon, Korea.
Abstract
- BACKGROUND
The use of several biochemical markers has improved the diagnosis of neonatal bacterial infection, which remains an important cause of morbidity and mortality. Recently, serum procalcitonin (PCT) has been investigated as a new marker for the detection of bacterial infection. The aim of this study was to assess the usefulness of PCT in early neonatal bacterial infection and compare the diagnostic utility of PCT with that of C-reactive protein (CRP).
METHODS
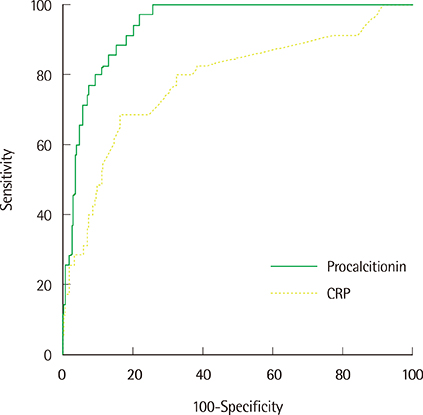
We retrospectively studied 216 neonates (109 full term, 107 preterm) whose PCT was measured 24 hr after birth. Thirty-five were clinically classified into an infected group, of which 17.4% had positive cultures. Clinical data, PCT, CRP, leukocyte, and neutrophil counts were evaluated. The diagnostic performance of PCT and CRP was studied using receiver operating characteristic analysis.
RESULTS
Compared to the non-infected group, the infected group displayed significantly higher median PCT (0.82 vs. 12.29 ng/mL, P<0.0001) and CRP (1.0 vs. 5.0 mg/L, P<0.0001) values, but similar leukocyte and neutrophil counts. The thresholds for PCT and CRP were 2.75 ng/mL (sensitivity, 97.1%; specificity, 76.7%) and 3.1 mg/L (sensitivity, 68.6%; specificity, 83.3%), respectively. The area under the curve for PCT was 0.937 (95% confidence interval [CI], 0.896-0.965) and 0.781 for CRP (95% CI, 0.720-0.834).
CONCLUSIONS
During the first 24 hr after birth, PCT is a more sensitive marker than CRP for bacterial infection and has predictive value for early neonatal bacterial infection.
MeSH Terms
Figure
Reference
-
1. Osrin D, Vergnano S, Costello A. Serious bacterial infections in newborn infants in developing countries. Curr Opin Infect Dis. 2004; 17:217–224.
Article2. Craig JC, Williams GJ, Jones M, Codarini M, Macaskill P, Hayen A, et al. The accuracy of clinical symptoms and signs for the diagnosis of serious bacterial infection in young febrile children: prospective cohort study of 15781 febrile illnesses. BMJ. 2010; 340:c1594.3. Gerdes JS. Diagnosis and management of bacterial infections in the neonate. Pediatr Clin North Am. 2004; 51:939–959.
Article4. Van den Bruel A, Thompson MJ, Haj-Hassan T, Stevens R, Moll H, Lakhanpaul M, et al. Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. BMJ. 2011; 342:d3082.
Article5. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993; 341:515–518.
Article6. Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004; 39:206–217.
Article7. Galetto-Lacour A, Zamora SA, Andreola B, Bressan S, Lacroix L, Da Dalt L, et al. Validation of a laboratory risk index score for the identification of severe bacterial infection in children with fever without source. Arch Dis Child. 2010; 95:968–973.
Article8. Chiesa C, Panero A, Rossi N, Stegagno M, De Giusti M, Osborn JF, et al. Reliability of procalcitonin concentrations for the diagnosis of sepsis in critically ill neonates. Clin Infect Dis. 1998; 26:664–672.
Article9. Sachse C, Dressler F, Henkel E. Increased serum procalcitonin in newborn infants without infection. Clin Chem. 1998; 44:1343–1344.
Article10. Chiesa C, Natale F, Pascone R, Osborn JF, Pacifico L, Bonci E, et al. C reactive protein and procalcitonin: reference intervals for preterm and term newborns during the early neonatal period. Clin Chim Acta. 2011; 412:1053–1059.
Article11. Harbarth S, Holeckova K, Froidevaux C, Pittet D, Ricou B, Grau GE, et al. Diagnostic value of procalcitonin, interleukin-6 and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med. 2001; 164:396–402.
Article12. Altunhan H, Annagür A, Örs R, Mehmetoğlu I. Procalcitonin measurement at 24 hours of age may be helpful in the prompt diagnosis of early-onset neonatal sepsis. Int J Infect Dis. 2011; 15:e854–e858.13. Nnanna II, Ehis OJ, Sidiquo II, Nnanna IG, Adekunle O. Serum procalcitonin: Early detection of neonatal bacteremia and septicemia in a tertiary healthcare facility. N Am J Med Sci. 2011; 3:157–160.
Article14. Kim EK, Lee BS, Lee JA, Jo HS, Park JD, Kim BI, et al. Clinical availability of serum procalcitonin level in the diagnosis of neonatal bacterial infection. J Korean Soc Neonatol. 2001; 8:211–221.15. Franz AR, Kron M, Pohlandt F, Steinbach G. Comparison of procalcitonin with interleukin 8, C-reactive protein and differential white blood cell count for the early diagnosis of bacterial infections in newborn infants. Pediatr Infect Dis J. 1999; 18:666–671.
Article16. Kordek A, Halasa M, Podraza W. Early detection of an early onset infection in the neonate based on measurements of procalcitonin and C-reactive protein concentrations in cord blood. Clin Chem Lab Med. 2008; 46:1143–1148.
Article17. Fernández Lopez A, Luaces Cubells C, García García JJ, Fernández Pou J. Procalcitonin in pediatric emergency departments for the early diagnosis of invasive bacterial infections in febrile infants: results of a multicenter study and utility of a rapid qualitative test for this marker. Pediatr Infect Dis J. 2003; 22:895–903.
Article18. Andreola B, Bressan S, Callegaro S, Liverani A, Plebani M, Da Dalt L. Procalcitonin and C-reactive protein as diagnostic markers of severe bacterial infections in febrile infants and children in the emergency department. Pediatr Infect Dis J. 2007; 26:672–677.
Article19. Hofer N, Resch R. CRP in term and preterm newborns. Clin Chim Acta. 2011; 412:1888.
Article20. Turner D, Hammerman C, Rudensky B, Schlesínger Y, Goia C, Schimmel MS. Procalcitonin in preterm infants during the first few days of life: introducing an age related nomogram. Arch Dis Child Fetal Neonatal Ed. 2006; 91:F283–F286.
Article21. Lapillonne A, Basson E, Monneret G, Bienvenu J, Salle BL. Lack of specificity of procalcitonin for sepsis diagnosis in premature infants. Lancet. 1998; 351:1211–1212.
Article22. Bender L, Thaarup J, Varming K, Krarup H, Ellermann-Eriksen S, Ebbesen F. Early and late markers for the detection of early-onset neonatal sepsis. Dan Med Bull. 2008; 55:219–223.23. Yu Z, Liu J, Sun Q, Qiu Y, Han S, Guo X. The accuracy of the procalcitonin test for the diagnosis of neonatal sepsis: a meta-analysis. Scand J Infect Dis. 2010; 42:723–733.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Availability of Serum Procalcitonin Level in the Diagnosis of Neonatal Bacterial Infection
- The Correlation between Infection Probability Score and Procalcitonin in Emergency Department Patients
- Serum Procalcitonin Level Reflects the Severity of Cellulitis
- The influencing factors on procalcitonin values in newborns with noninfectious conditions during the first week of life
- Procalcitonin as a Predictive Factor for the Clinical Outcome of Patients with Coronavirus Disease 2019