Lab Med Online.
2013 Apr;3(2):104-109.
A Case of Hepatosplenic T-cell Lymphoma Diagnosed by Bone Marrow Examination
- Affiliations
-
- 1Department of Laboratory Medicine, Korea Cancer Center Hospital, Korea Institute of Radiological & Medical Sciences, Seoul, Korea. hicyh@paran.com
- 2Department of Internal Medicine, Korea Cancer Center Hospital, Korea Institute of Radiological & Medical Sciences, Seoul, Korea.
- 3Department of Pathology, Korea Cancer Center Hospital, Korea Institute of Radiological & Medical Sciences, Seoul, Korea.
Abstract
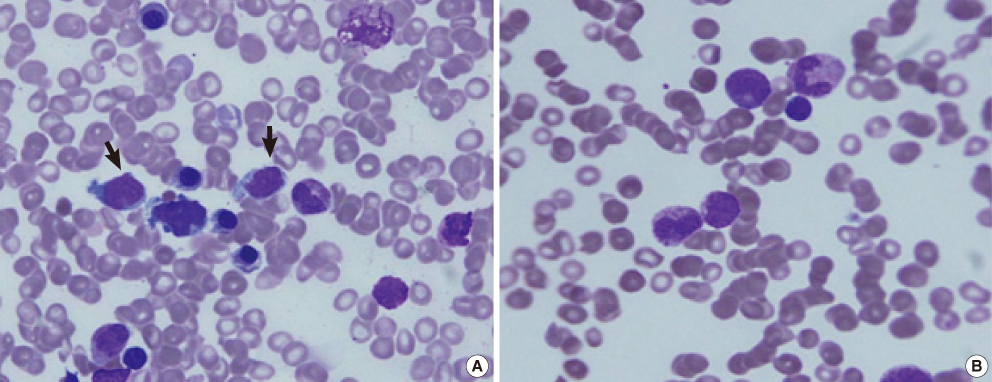
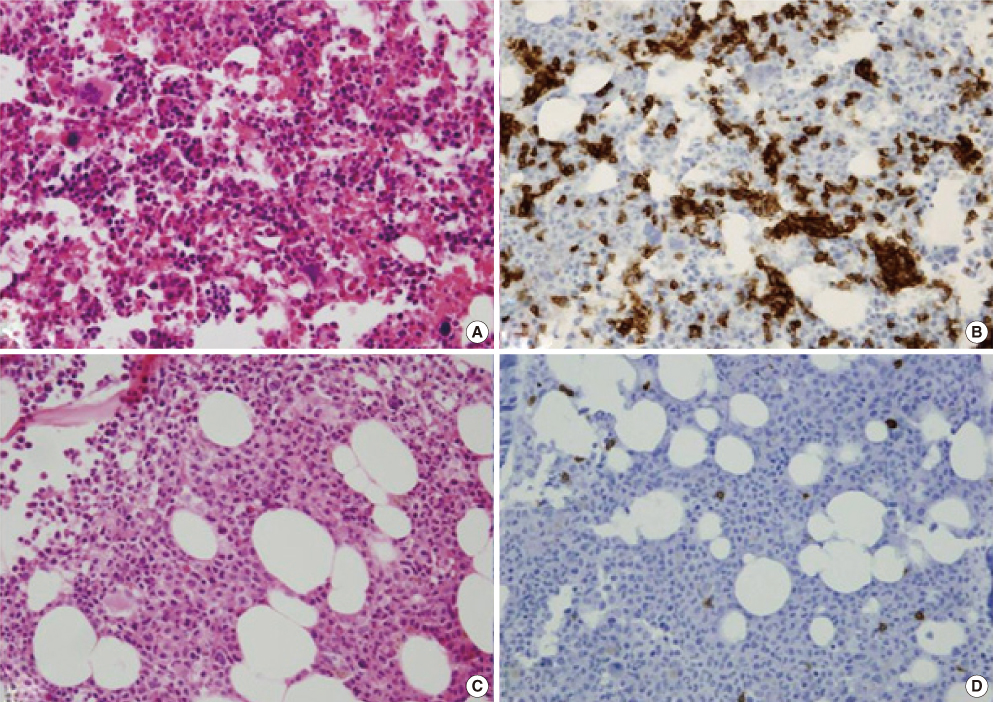
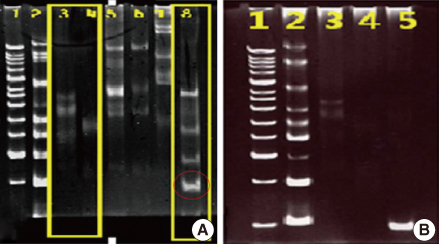
- Hepatosplenic T-cell lymphoma (HSTL) is a condition in which lymphoma cells infiltrate the sinusoids of the liver, spleen, and bone marrow, without lymph node involvement. We encountered a case of hepatosplenic T-cell lymphoma in a Vietnamese woman. The patient was hospitalized with epigastric pain and nausea. Splenomegaly and multiple poorly defined, low-attenuating nodular lesions in the liver were visualized on computed tomography (CT), and thrombocytopenia was noted. The lymph nodes were not significantly enlarged. Splenic biopsy could not be performed because of severe thrombocytopenia. Neoplastic lymphoid cells were present in bone marrow aspirates. Bone marrow sections revealed infiltration of CD3(+) and CD20(-) neoplastic lymphoid cells in the sinusoids. A clonality assay (IdentiClone T-Cell Receptor Delta Gene Clonality Assay; Invivoscribe Technologies, USA) showed gene rearrangements in the T-cell receptor delta gene. Thus, we made a confirmatory diagnosis of HSTL. When splenic biopsy is not available, bone marrow aspirates and clonality assessment may become useful diagnostic tools.
MeSH Terms
Figure
Reference
-
1. Swerdlow SH, Campo E, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 2008. 4th ed. Lyon, France: IARC Press;292–293.2. Cooke CB, Krenacs L, Stetler-Stevenson M, Greiner TC, Raffeld M, Kingma DW, et al. Hepatosplenic T-cell lymphoma: a distinct clinicopathologic entity of cytotoxic gamma delta T-cell origin. Blood. 1996. 88:4265–4274.
Article3. Weidmann E. Hepatosplenic T cell lymphoma. A review on 45 cases since the first report describing the disease as a distinct lymphoma entity in 1990. Leukemia. 2000. 14:991–997.
Article4. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, et al. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood. 1994. 84:1361–1392.
Article5. Armitage JO. The aggressive peripheral T-cell lymphomas: 2012 Update on diagnosis, risk stratification, and management. Am J Hematol. 2012. 87:511–519.
Article6. Park IG, Suh CW, Hur JR, Kim SJ, Park KU, Park SJ, et al. A case of a young woman with hepatosplenic gamma delta T-cell lymphoma. Cancer Res Treat. 2001. 33:264–268.
Article7. Lee SK, Woo HY, Park Q, Kim SH, Lee HG, Ko YH. A case of bone marrow involvement hepatosplenic γδ T-cell lymphoma. Korean J Hematol. 2002. 37:134–137.8. Lee YS, Kim HJ, Park SH, Cho YK, Jeon WK, Kim BI, et al. A case of hepatosplenic T-cell lymphoma mimicking a hemochromatosis. Korean J Med. 2006. 70:151–155.9. Kim SB, Jeong SH, Park JH, Kim HS, Kim B, Lee HS, et al. A Case of successful allogeneic stem cell transplantation for chemotherapy-refractory hepatosplenic γδ-T cell lymphoma. Korean J Hematol. 2009. 44:284–288.
Article10. Jeon BS, Lee YJ, Jeon SE, Park SS, Lim YT, Lee EY, et al. An adolescent case of hepatosplenic T-cell lymphoma. Clin Pediatr Hematol Oncol. 2010. 17:204–208.11. Choi JY, Park HS, Han DS, Kim JH, Hyun YS, Bae JH, et al. A case of hepatosplenic T-cell lymphoma with colonic involvement. Intest Res. 2011. 9:51–56.
Article12. Belhadj K, Reyes F, Farcet JP, Tilly H, Bastard C, Angonin R, et al. Hepatosplenic γδ T-cell lymphoma is a rare clinicopathologic entity with poor outcome: report on a series of 21 patients. Blood. 2003. 102:4261–4269.
Article13. Farcet JP, Gaulard P, Marolleau JP, Le Couedic JP, Henni T, Gourdin MF, et al. Hepatosplenic T-cell lymphoma: sinusal/sinusoidal localization of malignant cells expressing the T-cell receptor γδ. Blood. 1990. 75:2213–2219.
Article14. Wang CC, Tien HF, Lin MT, Su IJ, Wang CH, Chuang SM. Consistent presence of isochromosome 7q in hepatosplenic T gamma/delta lymphoma: a new cytogenetic-clinicopathologic entity. Genes Chromosomes Cancer. 1995. 12:161–164.
Article15. Jonveaux P, Daniel MT, Martel V, Maarek O, Berger R. Isochromosome 7q and trisomy 8 are consistent primary, non-random chromosomal abnormalities associated with hepatosplenic T gamma/delta lymphoma. Leukemia. 1996. 10:1453–1455.16. Alonsozana EL, Stamberg J, Kumar D, Jaffe ES, Medeiros LJ, Frantz C. Isochromosome 7q: the primary cytogenetic abnormality in hepatosplenic gammadelta T cell lymphoma. Leukemia. 1997. 11:1367–1372.
Article17. Herrinton LJ, Liu L, Abramson O, Jaffe ES. The incidence of hepatosplenic T-cell lymphoma in a large managed care organization, with reference to anti-tumor necrosis factor therapy, Northern California, 2000-2006. pharmacoepidemiol Drug Saf. 2012. 21:49–52.
Article18. Beigel F, Jürgens M, Tillack C, Subklewe M, Mayr D, Göke B, et al. Hepatosplenic T-cell lymphoma in a patient with Crohn's disease. Nat Rev Gastroenterol Hepatol. 2009. 6:433–436.
Article19. Kandiel A, Fraser AG, Korelitz BI, Brensinger C, Lewis JD. Increased risk of lymphoma among inflammatory bowel disease patients treated with azathioprine and 6-mercaptopurine. Gut. 2005. 54:1121–1125.
Article20. Mackey AC, Green L, Liang LC, Dinndorf P, Avigan M. Hepatosplenic T cell lymphoma associated with infliximab use in young patients treated for inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2007. 44:265–267.
Article21. Niitsu N, Kohri M, Togano T, Nakamine H, Nakamura S, Iwabuchi K, et al. Development of hepatosplenic γδ T-cell lymphoma with pancytopenia during early pregnancy: a case report and review of the literature. Eur J Haematol. 2004. 73:367–371.
Article22. Glaser M, Goropevšek A, Kavalar R, Glaser A. Hepatosplenic gamma-delta T-cell lymphoma in a female patient after delivery. Hematology Reports. 2012. 4:e4.
Article23. Das R, Sachdeva MU, Malhotra P, Das A, Ahluwalia J, Bal A, et al. Diagnostic Difficulties of Pure Intrasinusoidal bone marrow infiltration of non-Hodgkin's lymphoma: A report of eight cases from India. Jpn J Clin Oncol. 2011. 41:1303–1307.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Adolescent Case of Hepatosplenic T-cell Lymphoma
- A Case of Bone Marrow Involvement of Hepatosplenic gamma delta-Cell Lymphoma
- Sinusoidal infiltration of hepatosplenic lymphoma in liver and bone marrow
- A Case of Successful Allogeneic Stem Cell Transplantation for Chemotherapy-refractory Hepatosplenic gamma delta-T Cell Lymphoma
- Hepatosplenic B-cell lymphoma associated with hemophagocytic syndrome: a case report