Lab Med Online.
2012 Oct;2(4):197-203.
Diagnostic Usefulness of Basic Hematologic Tests for the Detection of Bacteremia in Febrile Patients with Neutrophilia
- Affiliations
-
- 1Department of Laboratory Medicine, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea. rhcpyoung@hanmail.net
- 2Department of Internal Medicine, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea.
Abstract
- BACKGROUND
Alterations in blood cell count are well recognized features of bacteremia. The study objective was to determine the hematologic changes predictive of bacteremia.
METHODS
We retrospectively studied febrile adult patients with neutrophilia and included patients were either bacteriologically proven cases or those who had clinically suspected bacterial infections. Hematologic findings derived from basic hematologic tests were compared between patients with and those without bacteremia.
RESULTS
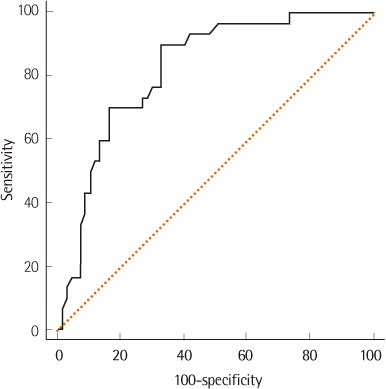
Of the 624 patients, 143 (22.9%) had significant bacteremia. The following items were significantly different between patients with and those without bacteremia by univariate analysis: absolute neutrophil count, neutrophil differential, absolute lymphocyte count, lymphocyte differential, platelet count and band-associated parameters such as absolute band neutrophil count (ABC). Multivariate analysis revealed platelet count, lymphocyte differential and ABC as independent predictors (P<0.0001, each). Platelet count, the most potent predictor of bacteremia, showed area under the curve (AUC) of 0.685. Analysis according to the primary diagnosis indicated that the most potent predictors of bacteremia in patients with respiratory tract, urinary tract and hepatobiliary system infections were platelet count (P=0.002, AUC=0.697), ABC (P=0.002, AUC=0.681) and neutrophil differential (P=0.0001, AUC=0.822), respectively.
CONCLUSIONS
Simple variables obtained from basic hematologic tests were associated with bacteremia even in febrile patients with neutrophilia. In particular, very high neutrophil differential was highly predictive of bacteremia in patients with hepatobiliary system infections and its clinical usefulness needs to be elucidated in a prospective study.
Keyword
MeSH Terms
Figure
Reference
-
1. Paolucci M, Landini MP, Sambri V. Conventional and molecular techniques for the early diagnosis of bacteraemia. Int J Antimicrob Agents. 2010. 36:Suppl 2. S6–S16.
Article2. Bates DW, Lee TH. Rapid classification of positive blood cultures. Prospective validation of a multivariate algorithm. JAMA. 1992. 267:1962–1966.
Article3. Groeneveld AB, Bossink AW, van Mierlo GJ, Hack CE. Circulating inflammatory mediators in patients with fever: predicting bloodstream infection. Clin Diagn Lab Immunol. 2001. 8:1189–1195.
Article4. Jaimes F, Arango C, Ruiz G, Cuervo J, Botero J, Vélez G, et al. Predicting bacteremia at the bedside. Clin Infect Dis. 2004. 38:357–362.
Article5. Raz R, Ben-Israel Y, Gronich D, Granot E, Colodner R, Visotzky I. Usefulness of blood cultures in the management of febrile patients in long-term care facilities. Eur J Clin Microbiol Infect Dis. 2005. 24:745–748.
Article6. Nakamura T, Takahashi O, Matsui K, Shimizu S, Setoyama M, Nakagawa M, et al. Clinical prediction rules for bacteremia and in-hospital death based on clinical data at the time of blood withdrawal for culture: an evaluation of their development and use. J Eval Clin Pract. 2006. 12:692–703.
Article7. Shapiro NI, Wolfe RE, Wright SB, Moore R, Bates DW. Who needs a blood culture? A prospectively derived and validated prediction rule. J Emerg Med. 2008. 35:255–264.
Article8. Peduzzi P, Shatney C, Sheagren J, Sprung C. The Veterans Affairs Systemic Sepsis Cooperative Study Group. Predictors of bacteremia and gram-negative bacteremia in patients with sepsis. Arch Intern Med. 1992. 152:529–535.
Article9. Fontanarosa PB, Kaeberlein FJ, Gerson LW, Thomson RB. Difficulty in predicting bacteremia in elderly emergency patients. Ann Emerg Med. 1992. 21:842–848.
Article10. Pfitzenmeyer P, Decrey H, Auckenthaler R, Michel JP. Predicting bacteremia in older patients. J Am Geriatr Soc. 1995. 43:230–235.
Article11. Wyllie DH, Bowler IC, Peto TE. Relation between lymphopenia and bacteraemia in UK adults with medical emergencies. J Clin Pathol. 2004. 57:950–955.
Article12. Yoshida T, Tsushima K, Tsuchiya A, Nishikawa N, Shirahata K, Kaneko K, et al. Risk factors for hospital-acquired bacteremia. Intern Med. 2005. 44:1157–1162.
Article13. Abidi K, Khoudri I, Belayachi J, Madani N, Zekraoui A, Zeggwagh AA, et al. Eosinopenia is a reliable marker of sepsis on admission to medical intensive care units. Crit Care. 2008. 12:R59.
Article14. Wibrow BA, Ho KM, Flexman JP, Keil AD, Kohrs DL. Eosinopenia as a diagnostic marker of bloodstream infection in hospitalized paediatric and adult patients: a case-control study. Anaesth Intensive Care. 2011. 39:224–230.
Article15. Park DH, Park K, Park J, Park HH, Chae H, Lim J, et al. Screening of sepsis using leukocyte cell population data from the Coulter automatic blood cell analyzer DxH800. Int J Lab Hematol. 2011. 33:391–399.
Article16. Williams J, Bellamy R. Fever of unknown origin. Clin Med. 2008. 8:526–530.
Article17. Hoffbrand AV, Moss PAH, editors. Essential Haematology. 2006. 5th ed. Oxford: Blackwell Publishing Ltd.;101–104.18. Sekhon SS, Roy V. Thrombocytopenia in adults: a practical approach to evaluation and management. South Med J. 2006. 99:491–498.
Article19. Afessa B, Greaves WL, Frederick WR. Pneumococcal bacteremia in adults: a 14-year experience in an inner-city university hospital. Clin Infect Dis. 1995. 21:345–351.
Article20. Watanakunakorn C, Bailey TA. Adult bacteremic pneumococcal pneumonia in a community teaching hospital, 1992-1996. A detailed analysis of 108 cases. Arch Intern Med. 1997. 157:1965–1971.
Article21. Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005. 128:3854–3862.
Article22. Leung WS, Chu CM, Tsang KY, Lo FH, Lo KF, Ho PL. Fulminant community-acquired Acinetobacter baumannii pneumonia as a distinct clinical syndrome. Chest. 2006. 129:102–109.
Article23. Aliberti S, Amir A, Peyrani P, Mirsaeidi M, Allen M, Moffett BK, et al. Incidence, etiology, timing, and risk factors for clinical failure in hospitalized patients with community-acquired pneumonia. Chest. 2008. 134:955–962.
Article24. Hsu CY, Fang HC, Chou KJ, Chen CL, Lee PT, Chung HM. The clinical impact of bacteremia in complicated acute pyelonephritis. Am J Med Sci. 2006. 332:175–180.
Article25. Bahagon Y, Raveh D, Schlesinger Y, Rudensky B, Yinnon AM. Prevalence and predictive features of bacteremic urinary tract infection in emergency department patients. Eur J Clin Microbiol Infect Dis. 2007. 26:349–352.
Article26. Farinon AM, Grande M, Torquati A, D'Antini P. Multivariate analysis for predicting the presence of bacteria in bile in patients with acute cholecystitis. Eur J Surg. 1993. 159:531–534.27. Tsai MJ, Chen JD, Tiu CM, Chou YH, Hu SC, Chang CY. Can acute cholecystitis with gallbladder perforation be detected preoperatively by computed tomography in ED? Correlation with clinical data and computed tomography features. Am J Emerg Med. 2009. 27:574–581.
Article28. Derici H, Kara C, Bozdag AD, Nazli O, Tansug T, Akca E. Diagnosis and treatment of gallbladder perforation. World J Gastroenterol. 2006. 12:7832–7836.
Article29. Huang CC, Lo HC, Tzeng YM, Huang HH, Chen JD, Kao WF, et al. Percutaneous transhepatic gall bladder drainage: a better initial therapeutic choice for patients with gall bladder perforation in the emergency department. Emerg Med J. 2007. 24:836–840.
Article30. Aminzadeh Z, Parsa E. Relationship between age and peripheral white blood cell count in patients with sepsis. Int J Prev Med. 2011. 2:238–242.31. Limper M, de Kruif MD, Duits AJ, Brandjes DP, van Gorp EC. The diagnostic role of procalcitonin and other biomarkers in discriminating infectious from non-infectious fever. J Infect. 2010. 60:409–416.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Procalcitonin and C-Reactive Protein as Early Diagnostic Markers of Bacteremia in Cancer Patients with Febrile Neutropenia
- Febrile Illness with Skin Rashes
- The Risk Factor of Bacteremia in Children with Febrile Neutropenia due to Chemotherapy
- Clinical Manifestations of Febrile Neutropenic Patients with Solid Tumor and Risk Factors for Gram Positive Bacteremia
- Antibiotic-Resistant Gram-Negative Bacteremia in Febrile Neutropenic Children