Korean J Urol.
2008 Jan;49(1):88-91.
Comparison between Conventional and Microsurgical Testicular Sperm Extraction in Non-obstructive Azoospermia
- Affiliations
-
- 1Department of Urology, Kwandong University College of Medicine, Seoul, Korea. jtandro@cgh.co.kr
- 2Department of Urology, Mizmedi Hospital, Seoul, Korea.
Abstract
-
PURPOSE: Recovery of the testicular spermatozoa in non-obstructive azoospermic patients after intracytoplasmic sperm injection(ICSI) is a recent advance in the treatment of male infertility. In this study we compared sperm retrieval using microsurgical testicular sperm extraction(TESE) with retrieval by conventional TESE.
MATERIALS AND METHODS
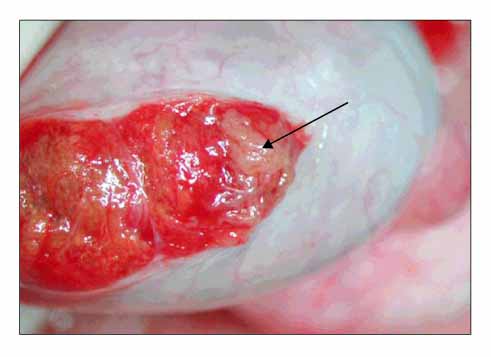
A total of 450 men with non-obstructive azoospermia were included in the study. 277 of these 450 men underwent conventional TESE(Group 1), and the other 173 patients underwent microsurgical TESE(Group 2). Microsurgical TESE was performed by making multiple incisions in the tunica albuginea under surgical microscopy, with avoiding the underlying testicular artery. The seminiferous tubules that appeared dilated and opaque were harvested. The cases were categorized into three groups, that is, the germ cell aplasia group, the maturation arrest group and the hypospermatogenesis group. The sperm retrieval rates for the patients in the three histopathological categories were compared between the two groups.
RESULTS
The sperm retrieval rate by conventional TESE was 30.7% and it was 31.4% by microsurgical TESE(p=0.938). For the cases of histologically diagnosed germ cell aplasia the retrieval rate was 11.6% and 21.2%, respectively, for group 1 and group 2(p=0.026). For the cases of maturation arrest the retrieval rate was 24.4% and 26.0%, respectively, for group 1 and group 2(p=0.884). For the cases of hypospermatogenesis the retrieval rate was 83.0% and 91.3%, respectively, for group 1 and group 2(p=0.339).
CONCLUSIONS
For non-obstructive patients, and especially those with germ cell aplasia, microsurgical TESE can effectively retrieve spermatozoa and minimize the risk of complication.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim WT, Seo JT. Outcome of microsurgical multiple testicular sperm extraction for patients with Y chromosome microdeletion. Korean J Urol. 2005. 46:819–822.2. Dubin L, Amelar RD. Etiologic factors in 1294 consecutive cases of male infertility. Fertil Steril. 1971. 22:469–474.3. Schoysman R, Vanderzwalmen P, Nijs M, Segal L, Segal-Bertin G, Geerts L, et al. Pregnancy after fertilisation with human testicular spermatozoa. Lancet. 1993. 342:1237.4. Seo JT, Ko WJ. Predictive factors of successful testicular sperm recovery in non-obstructive azoospermia patients. Int J Androl. 2001. 24:306–310.5. Ostad M, Liotta D, Ye Z, Schlegel PN. Testicular sperm extraction for nonobstructive azoospermia: results of a multibiopsy approach with optimized tissue dispersion. Urology. 1998. 52:692–696.6. Silber SJ. Microsurgical TESE and the distribution of spermatogenesis in non-obstructive azoospermia. Hum Reprod. 2000. 15:2278–2284.7. Silber SJ, Van Steirteghem AC, Liu J, Nagy Z, Tournaye H, Devroey P. High fertilization and pregnancy rate after intracytoplasmic sperm injection with spermatozoa obtained from testicle biopsy. Hum Reprod. 1995. 10:148–152.8. Seo JT, Park YS, Kim JH, Lee YS, Jun JH, Lee HJ, et al. The treatment of non-obstructive azoospermia. Korean J Fetil Steril. 1997. 24:95–99.9. Van Steirteghem AC, Nagy Z, Joris H, Liu J, Staessen C, Smitz J, et al. High fertilization and implantation rates after intracytoplasmic sperm injection. Hum Reprod. 1993. 8:1061–1066.10. Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992. 340:17–18.11. Devroey P, Liu J, Nagy Z, Goossens A, Tournaye H, Camus M, et al. Pregnancies after testicular sperm extraction and intracytoplasmic sperm injection in non-obstructive azoospermia. Hum Reprod. 1995. 10:1457–1460.12. Tournaye H, Camus M, Goossens A, Liu J, Nagy P, Silber S, et al. Recent concepts in the management of infertility because of non-obstructive azoospermia. Hum Reprod. 1995. 10:Suppl 1. 115–119.13. Tournaye H, Verheyen G, Nagy P, Ubaldi F, Goossens A, Silber S, et al. Are there any predictive factors for successful testicular sperm recovery in azoospermic patients? Hum Reprod. 1997. 12:80–86.14. Okada H, Dobashi M, Yamazaki T, Hara I, Fujisawa M, Arakawa S, et al. Conventional versus microdissection testicular sperm extraction for nonobstructive azoospermia. J Urol. 2002. 168:1063–1067.15. Schlegel PN. Testicular sperm extraction: microdissection improves sperm yield with minimal tissue excision. Hum Reprod. 1999. 14:131–135.16. Tsujimura A, Matsumiya K, Miyagawa Y, Tohda A, Miura H, Nishimura K, et al. Conventional multiple or microdissection testicular sperm extraction a comparative study. Hum Reprod. 2002. 17:2924–2929.17. Ramasamy R, Yagan N, Schilegel PN. Structural and functional changes to the testis after conventional versus microdissection testicular sperm extraction. Urology. 2005. 65:1190–1194.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Meaning Touch Imprint and Testicular Sperm Extraction(TEST) in Azoospermia Patients during Testis Biopsy
- Investigations on the Factors Predicting the Results of Testis Sperm Extraction
- The treatment of Non-obstructive Azoospermia
- Intracytoplasmic Sperm Injection with Testicular Sperm Extration in Obstructive Azoospermia
- Intracytoplasmic Sperm Injection with Testicular Sperm Extraction in Patients with Obstructive and Non-obstructive Azoospermia