Korean J Urol.
2008 Apr;49(4):320-324.
The Factor Affecting Radical Retropubic Prostatectomy: The Bony Pelvic Shape Imaged by Magnetic Resonance Imaging
- Affiliations
-
- 1Department of Urology, Chonnam National University Medical School, Gwangju, Korea. sbryu@chonnam.ac.kr
Abstract
-
PURPOSE: We investigated how the bony pelvic shape, as imaged by preoperative magnetic resonance imaging(MRI), affects radical retropubic prostatectomy(RRP).
MATERIALS AND METHODS
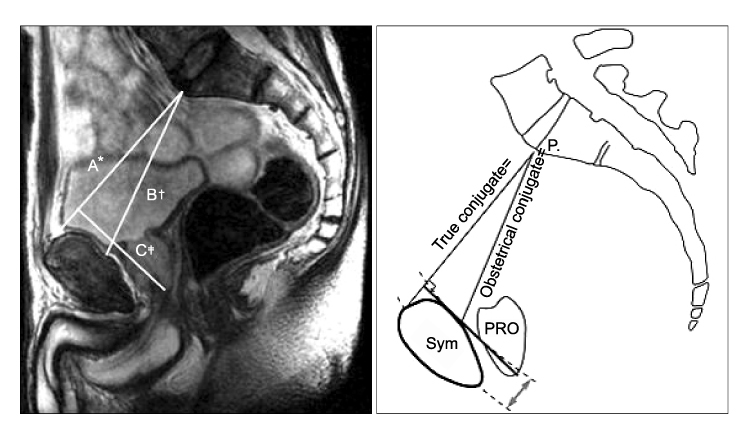
We investigated 27 patients who underwent radical prostatectomy between January 2004 and December 2006 in our hospital. We obtained images of their pelvic bone size on the sagittal plane by performing pelvic MRI. We measured the true conjugate diameter, the obstetric conjugate diameter and the difference between the former and the latter. In addition, we examined the age, body mass index(BMI), prostate-specific antigen(PSA), prostate volume, Gleason's score, pathologic stage, operative time, the estimated blood loss and the surgical margin involvement. We analyzed the factors that affected the estimated blood loss, operative time and surgical margin involvement by multiple linear regression analysis and multiple logistic regression analysis.
RESULTS
The mean age of the patients was 66.7+/-5.3 years, the true conjugate diameter and obsteric conjugate diameter were 105+/-8.9mm and 94.5+/-9.2 mm respectively, the difference of the diameters was 10.7+/-4.3mm, the BMI was 24.1+/-2.6kg/m(2), the PSA was 22.9+/-34.2ng/ml and the prostate volume was 33.7+/-14g. The estimated blood loss was 1,152.2+/-356.4cc, the operation time was 144.4+/-28.6 minutes and 8 patients had positive surgical margins. On the multiple linear regression analysis, the estimated blood loss increased 66cc in proportion to a 1mm difference between the true conjugate diameter and the obstetric conjugate diameter(p<0.001). The BMI was associated with the operative time on the multiple linear regression analysis(p=0.048).
CONCLUSIONS
For patients with RRP, the BMI was associated with the operative time. The estimated blood loss increased in proportion to the difference between the true conjugate diameter and the obstetric conjugate diameter, as measured by pelvic MRI before operation. We suggest that the symphyseal surface variability can be the one of the factors that affects the degree of operative difficulty.
MeSH Terms
Figure
Reference
-
1. Hsu EI, Hong EK, Lepor H. Influence of body weight and prostate volume on intraoperative, perioperative, and postoperative outcomes after radical retropubic prostatectomy. Urology. 2003. 61:601–606.2. Chang SS, Duong DT, Wells N, Cole EE, Smith JA Jr, Cookson MS. Predicting blood loss and transfusion requirements during radical prostatectomy: the significant negative impact of increasing body mass index. J Urol. 2004. 171:1861–1865.3. Freedland SJ, Grubb KA, Yiu SK, Nielsen ME, Mangold LA, Isaacs WB, et al. Obesity and capsular incision at the time of open retropubic radical prostatectomy. J Urol. 2005. 174:1798–1801.4. Brown JA, Rodin DM, Lee B, Dahl DM. Laparoscopic radical prostatectomy and body mass index: an assessment of 151 sequential cases. J Urol. 2005. 173:442–445.5. Ahlering TE, Eichel L, Edwards R, Skarecky DW. Impact of obesity on clinical outcomes in robotic prostatectomy. Urology. 2005. 65:740–744.6. Colcher AE, Sussman W. A practical technique for roentgen pelvimetry with a new positioning. AJR Am J Roentgenol. 1944. 51:207–214.7. Sporri S, Hanggi W, Braghetti A, Vock P, Schneider H. Pelvimetry by magnetic resonance imaging as a diagnostic tool to evaluate dystocia. Obstet Gynecol. 1997. 89:902–908.8. Stark DD, McCarthy SM, Filly RA, Parer JT, Hricak H, Callen PW. Pelvimetry by magnetic resonance imaging. AJR Am J Roentgenol. 1985. 144:947–950.9. Coakley FV, Eberhardt S, Wei DC, Wasserman ES, Heinze SB, Scardino PT, et al. Blood loss during radical retropubic prostatectomy: relationship to morphologic features on preoperative endorectal magnetic resonance imaging. Urology. 2002. 59:884–888.10. Hodroff MA, Stolpen AH, Denson MA, Bolinger L, Dreder KJ. Dynamic magnetic resonance imaging of the female pelvis: the relationship with the pelvic orgarn prolapse quantification staging system. J Urol. 2002. 167:1353–1355.11. Singh A, Fagin R, Shah G, Shekarriz B. Impact of prostate size and body mass index on perioperative morbidity after laparoscopic radical prostatectomy. J Urol. 2005. 173:552–554.12. Hong SK, Chang IH, Han BK, Yu JH, Han JH, Jeong SJ, et al. Impact of variations in bony pelvic dimensions on performing radical retropubic prostatectomy. Urology. 2007. 69:907–911.13. Emerson RE, Koch MO, Jones TD, Daggy JK, Juliar BE, Cheng L. The influence of extent of surgical margin positivity on prostate specific antigen recurrence. J Clin Pathol. 2005. 58:1028–1032.14. Freedland SJ, Aronson WJ, Kane CJ, Presti JC Jr, Amling CL, Elashoff D, et al. Impact of obesity on biochemical control after radical prostatectomy for clinically localized prostate cancer: a report by the Shared Equal Access Regional Cancer Hospital database study group. J Clin Oncol. 2004. 22:446–453.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Visible Angle on Magnetic Resonance Imaging Can Be Considered Indicator of Postoperative Outcome in Retropubic Radical Prostatectomy
- Preoperative Factors Predictive of Continence Recovery after Radical Retropubic Prostatectomy
- Factors Affecting the Outcome of Extraperitoneal Laparoscopic Radical Prostatectomy: Pelvic Arch Interference and Depth of the Pelvic Cavity
- Initial Experience of Three Cases of Radical Retropubic Prostatectomy
- Radical Prostatectomy