Korean J Urol.
2009 May;50(5):450-456.
The Prevalence and Management of Urinary Incontinence in Elderly Patients at Sanatorium in Busan Area
- Affiliations
-
- 1Department of Urology, Dong-A University School of Medicine, Busan, Korea. urogate@dau.ac.kr
Abstract
-
PURPOSE: Prevalence estimates and management methods for urinary incontinence among elderly patients aged 65 and over at sanatoriums in Busan area were investigated.
MATERIALS AND METHODS
A sample of 834 institutionalized patients was randomly selected from 13 sanatoriums with 100 and more beds in Busan. The study was designed as a cross-sectional study. Data were collected via face-to-face interviews using Appendix about general status, obstetric history, incontinence, and management method for incontinence. The survey was conducted from February to September 2008.
RESULTS
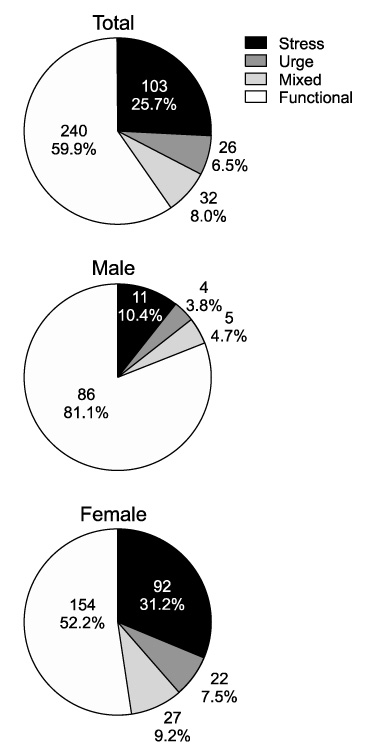
Overall prevalence of urinary incontinence in all of 834 respondents was found to be 48.1%: prevalences of stress incontinence, urge incontinence, mixed incontinence, and functional incontinence were 25.7%, 6.5%, 8.0% and 59.9%, respectively. Among the patients with urinary incontinence symptoms, 28.6% had associated-dermatologic problems.
CONCLUSIONS
The estimated prevalence of incontinence for elderly patients aged 65 and more cared at Sanatoriums in Busan area was 48.1%. However, systemic approaches in the management of urinary incontinence in such patients were lacking. Further efforts should be made for proper management of urinary incontinence among elderly patients cared at Sanatorium.
MeSH Terms
Figure
Reference
-
1. Korea National Statistical Office. Population projections for Korea. 2006. Seoul: Korean National Statistical Office.2. Korean Ministry of Health and Welfare. Yearbook on health and welfare statistics. 2007. 53rd ed. Seoul: Korean Ministry of Health and Welfare.3. Muscatello DJ, Rissel C, Szonyi G. Urinary symptoms and incontinence in an urban community: prevalence and associated factors in older men and women. Intern Med J. 2001. 31:151–160.4. Neil MR, Subbarao BY. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Geriatric incontinence and voiding dysfunction. Campbell-Walsh urology. 2006. 9th ed. Philadelphia: Saunders;2305–2321.5. Kim JS, Lee JZ. The prevalence of urinary incontinence in elderly women at institutionalized facilities in Pusan. Korean J Urol. 1999. 40:1019–1023.6. Tannenbaum C, DuBeau CE. Urinary incontinence in the nursing home: practical approach to evaluation and management. Clin Geriatr Med. 2004. 20:437–452.7. Levy R, Muller N. Urinary incontinence: economic burden and new choices in pharmaceutical treatment. Adv Ther. 2006. 23:556–573.8. Chiarelli P, Brown W, McElduff P. Leaking urine: prevalence and associated factors in Australian women. Neurourol Urodyn. 1999. 18:567–577.9. Oh SJ, Park WH, Park CH, Paick JS, Seo JT, Lee YS, et al. Prevalence of urinary incontinence and incontinence-related quality of life in Korean women: a population-based study. J Korean Continence Soc. 2003. 7:73–80.10. Offermans MP, Du Moulin MF, Hamers JP, Dassen T, Halfens RJ. Prevalence of urinary incontinence and associated risk factors in nursing home residents: a systematic review. Neurourol Urodyn. 2009. 28:288–294.11. Leary SM, Liu C, Cheesman AL, Ritter A, Tompson S, Greenwood R. Incontinence after brain injury: prevalence, outcome and multidisciplinary management on a neurological rehabilitation unit. Clin Rehabil. 2006. 20:1094–1099.12. Borrie MJ, Davidson HA. Incontinence in institutions: costs and contributing factors. CMAJ. 1992. 147:322–328.13. Hu TW, Kaltreider DL, Igou JF, Yu LC, Rohner TJ. Cost effectiveness of training incontinent elderly in nursing homes: a randomized clinical trial. Health Serv Res. 1990. 25:455–477.14. Schnelle JF, Newman DR, Fogarty T. Statistical quality control in nursing homes: assessment and management of chronic urinary incontinence. Health Serv Res. 1990. 25:627–637.15. Pinkowski PS. Prompted voiding in the long-term care facility. J Wound Ostomy Continence Nurs. 1996. 23:110–114.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The role of primary care of voiding dysfunction in rehabilitation and convalescent hospitals
- Incontinence Pad Usage in Medical Welfare Facilities in Korea
- Types of Male Incontinence and the Strategy for its Management
- Urinary incontinence and overactive bladder
- The Prevalence of Urinary Incontinence in Elderly Women at Institutionalized Facilities in Pusan