Ann Rehabil Med.
2016 Apr;40(2):341-350. 10.5535/arm.2016.40.2.341.
Effects of a Modified Hand Compression Bandage for Treatment of Post-Burn Hand Edemas
- Affiliations
-
- 1Department of Rehabilitation Medicine, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea. werch@hallym.or.kr
- 2Department of Rehabilitation Medicine, Hallym University Hangang Sacred Heart Hospital, Seoul, Korea.
- KMID: 2309935
- DOI: http://doi.org/10.5535/arm.2016.40.2.341
Abstract
OBJECTIVE
To evaluate the effect of a modified hand compression bandage in patients with a post-burn hand edema.
METHODS
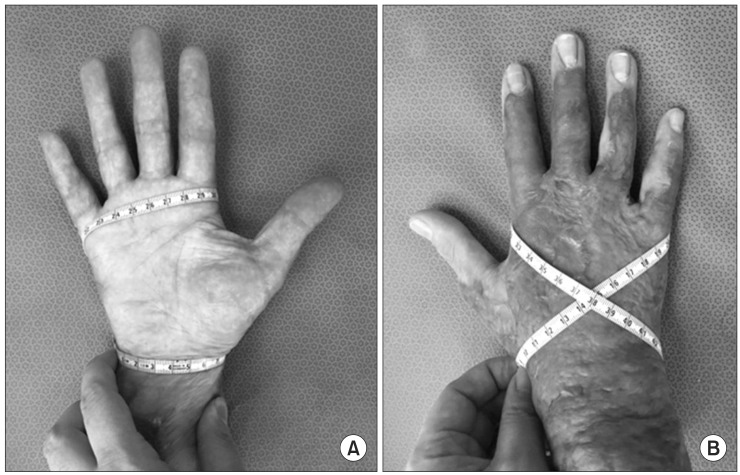
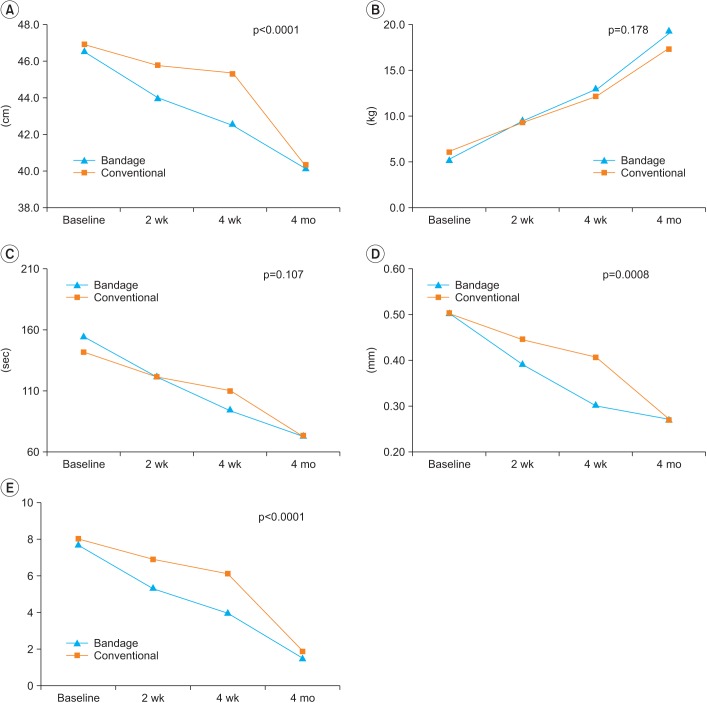
Patients were recruited from burn centers. We classified the patients into two groups: the modified hand compression bandage group comprising of 22 patients who had a modified hand compression bandage and received conventional physical therapy and the conventionally treated group, comprising of 20 patients who received only conventional physical therapy during the 4-week period post-burn. Hand circumference, hand skin thickness, and hand function were evaluated by grip strength, active range of motion (ROM), Jebsen hand function test, and visual analogue scale (VAS). These assessments were used to evaluate treatment effectiveness prior to the first treatment, 2 weeks after the first treatment, 4 weeks after the first treatment, and 4 months after the first treatment.
RESULTS
As a result of repeated-measures analysis of variance on hand circumference, skin thickness, VAS, and each metacarpophalangeal joint ROM, we found significant differences that corresponded to time effect (p<0.05) and time×group (reciprocal action) effect (p<0.05). The results of grasp power, Jebsen hand function test, and each proximal interphalangeal joint ROM, show significant differences in accordance with the time effect (p<0.05), however, there was no reciprocal action effect (p>0.05).
CONCLUSION
The modified hand compression bandage will be clinically useful for the treatment of patients with post-burn hand edemas.
Keyword
MeSH Terms
Figure
Reference
-
1. Smith MA, Munster AM, Spence RJ. Burns of the hand and upper limb: a review. Burns. 1998; 24:493–505. PMID: 9776087.2. Richard R, Staley M, Miller S, Warden G. To splint or not to splint: past philosophy and present practice. Part I. J Burn Care Rehabil. 1996; 17:444–453. PMID: 8889870.3. Frontera W, DeLisa JA. DeLisa's physical medicine and rehabilitation. 5th ed. Philadelphia: Saunders;2010. p. 1125–1150.4. Moore ML, Dewey WS, Richard RL. Rehabilitation of the burned hand. Hand Clin. 2009; 25:529–541. PMID: 19801125.
Article5. Atiyeh BS, El Khatib AM, Dibo SA. Pressure garment therapy (PGT) of burn scars: evidence-based efficacy. Ann Burns Fire Disasters. 2013; 26:205–212. PMID: 24799851.6. Dewey WS, Hedman TL, Chapman TT, Wolf SE, Holcomb JB. The reliability and concurrent validity of the figure-of-eight method of measuring hand edema in patients with burns. J Burn Care Res. 2007; 28:157–162. PMID: 17211219.
Article7. Maihafer GC, Llewellyn MA, Pillar WJ Jr, Scott KL, Marino DM, Bond RM. A comparison of the figure-of-eight method and water volumetry in measurement of hand and wrist size. J Hand Ther. 2003; 16:305–310. PMID: 14605647.
Article8. Leard JS, Breglio L, Fraga L, Ellrod N, Nadler L, Yasso M, et al. Reliability and concurrent validity of the figure-of-eight method of measuring hand size in patients with hand pathology. J Orthop Sports Phys Ther. 2004; 34:335–340. PMID: 15233395.
Article9. Kang TD, Jang KE, Park DS, Kim SB, Jung EH. Ultrasonographic assessment of nonsurgical treatment of postburn hypertrophic scar. J Korean Acad Rehabil Med. 1999; 23:397–404.10. Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969; 50:311–319. PMID: 5788487.11. Choi JS, Mun JH, Lee JY, Jeon JH, Jung YJ, Seo CH, et al. Effects of modified dynamic metacarpophalangeal joint flexion orthoses after hand burn. Ann Rehabil Med. 2011; 35:880–886. PMID: 22506218.
Article12. Vincent G, Radha H. Burn rehabilitation. In : Braddom RL, editor. Physical medicine and rehabilitation. 4th ed. Philadelphia: Saunders;2011. p. 1403–1418.13. Lund T, Onarheim H, Reed RK. Pathogenesis of edema formation in burn injuries. World J Surg. 1992; 16:2–9. PMID: 1290261.
Article14. Li-Tsang CW, Feng B, Huang L, Liu X, Shu B, Chan YT, et al. A histological study on the effect of pressure therapy on the activities of myofibroblasts and keratinocytes in hypertrophic scar tissues after burn. Burns. 2015; 41:1008–1016. PMID: 25681960.
Article15. Salisbury RE, Loveless S, Silverstein P, Wilmore DW, Moylan JA Jr, Pruitt BA Jr. Postburn edema of the upper extremity: evaluation of present treatment. J Trauma. 1973; 13:857–862. PMID: 4774842.16. Ause-Ellias KL, Richard R, Miller SF, Finley RK Jr. The effect of mechanical compression on chronic hand edema after burn injury: a preliminary report. J Burn Care Rehabil. 1994; 15:29–33. PMID: 8150839.
Article17. Flowers KR. String wrapping versus massage for reducing digital volume. Phys Ther. 1988; 68:57–59. PMID: 3336619.
Article18. Laseter GF. Management of the stiff hand: a practical approach. Orthop Clin North Am. 1983; 14:749–765. PMID: 6634092.
Article19. Lowell M, Pirc P, Ward RS, Lundy C, Wilhelm DA, Reddy R, et al. Effect of 3M Coban Self-Adherent Wraps on edema and function of the burned hand: a case study. J Burn Care Rehabil. 2003; 24:253–258. PMID: 14501426.
Article20. Omar MT, El-Badawy AM, Borhan WH, Nossier A. Improvement of edema and hand function in superficial second degree hand burn using electrical stimulation. Egypt J Plast Reconstr Surg. 2004; 28:141–147.21. Edgar DW, Fish JS, Gomez M, Wood FM. Local and systemic treatments for acute edema after burn injury: a systematic review of the literature. J Burn Care Res. 2011; 32:334–347. PMID: 21252688.
Article22. Covey MH, Dutcher K, Heimbach DM, Marvin JA, Engrav LH, deLateur B. Return of hand function following major burns. J Burn Care Rehabil. 1987; 8:224–226. PMID: 3301862.
Article23. Kong Y, Sohn S, Han J. A review study for grip strengths of hand. J Ergon Soc Korea. 2010; 29:715–725.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Heterotopic Ossification in Post-Burn Scar Contracture of the Wrist
- Effects of Modified Dynamic Metacarpophalangeal Joint Flexion Orthoses after Hand Burn
- A Case of Crushing Burn Injury: A Case Report
- Immediate Fasciotomy for Acute Thermal Contact Burn Combined with Compression Injury of the Right Forearm and Hand: A Case Report
- Correction of hand deformities after burns