Korean J Women Health Nurs.
2015 Sep;21(3):161-170. 10.4069/kjwhn.2015.21.3.161.
Impact of a Lifestyle Modification Program on Menstrual Irregularity among Overweight or Obese Women with Polycystic Ovarian Syndrome
- Affiliations
-
- 1Woman's Health and Midwifery Nursing Department, Faculty of Nursing, Mansoura University, Egypt. tm_fathy@yahoo.com
- 2Obstetrics and Gynecology Department, Faculty of Medicine, Mansoura University, Egypt.
- 3Rheumatology and Rehabilitation Department, Faculty of Medicine, Mansoura University, Egypt.
- KMID: 2307913
- DOI: http://doi.org/10.4069/kjwhn.2015.21.3.161
Abstract
- PURPOSE
This study aimed to evaluate the impact of a lifestyle modification program on menstrual irregularity among overweight and obese women with polycystic ovarian syndrome.
METHODS
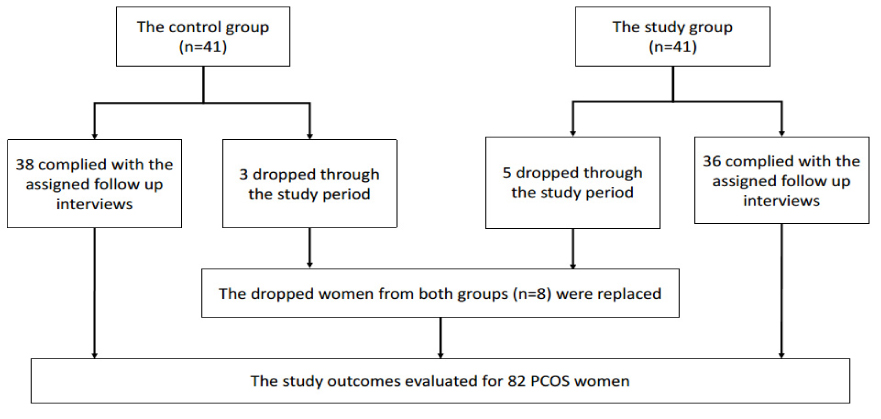
A quasi experimental research design was used to conduct this study on 82 women with polycystic ovarian syndrome at the Gynecology and Obesity clinics of Mansoura University Hospital, Egypt. Two groups were included; the study group received a lifestyle modification program for 48 weeks, while the control group was not subjected to this program. Data collection was done for the following variables, a structured interview questionnaire was used to assess the women's general characteristics, menstrual patterns, and 24-hour dietary recall and the researcher took anthropometric measurements and assessed hirsutism by the Ferriman-Gallwey scale.
RESULTS
After one year of lifestyle modification, the number of menstrual cycles significantly increased from 2.7+/-1.6 to 6.9+/-1.5 (t=12.26, p<.001) in the study group compared to insignificant minor changes among the control group (t=0.69, p=.488). Additionally, 58.5% were menstruating regularly compared to none in the control group (chi2=33.93, p<.001).
CONCLUSION
Participating in a lifestyle modification program was effective in reducing menstrual cycle's irregularity among overweight and obese women with PCOS. Thus, it is recommended to motivate the nurses in counseling the PCOS women on lifestyle modifications.
MeSH Terms
Figure
Reference
-
1. Ehrmann DA. Polycystic ovary syndrome. N Engl J Med. 2005; 352(12):1223–1236.
Article2. Abdelhafeez AT, Taha SA, Ahmad NA, Khalaf MR. Familial prevalence of PCOS and PCOS related features in Upper Egypt. Al-Azhar Assiut Med J. 2003; 1(3):1–8.3. Teede H, Deeks A, Moran L. Polycystic ovary syndrome: A complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010; 8:41.
Article4. Hoeger KM. Role of lifestyle modification in the management of polycystic ovary syndrome. Best Pract Res Clin Endocrinol Metab. 2006; 20(2):293–310.
Article5. Guzick DS, Wing R, Smith D, Berga SL, Winters SJ. Endocrine consequences of weight loss in obese, hyperandrogenic, anovulatory women. Fertil Steril. 1994; 61(4):598–604.6. Moran LJ, Brinkworth GD, Norman RJ. Dietary therapy in polycystic ovary syndrome. Semin Reprod Med. 2008; 26(1):85–92.
Article7. Galal OM. The nutrition transition in Egypt: Obesity, undernutrition and the food consumption context. Public Health Nutr. 2002; 5(1A):141–148.
Article8. Moran LJ, Lombard CB, Lim S, Noakes M, Teede HJ. Polycystic ovary syndrome and weight management. Womens Health (Lond Engl). 2010; 6(2):271–283.
Article9. Moran LJ, Hutchison SK, Norman RJ, Teede HJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011; (2):CD007506.
Article10. Fearnley EJ, Marquart L, Spurdle AB, Weinstein P, Webb PM. Polycystic ovary syndrome increases the risk of endometrial cancer in women aged less than 50 years: An Australian casecontrol study. Cancer Causes Control. 2010; 21(12):2303–2308.11. Ferriman D, Gallwey JD. Clinical assessment of body hair growth in women. J Clin Endocrinol Metab. 1961; 21:1440–1447.
Article12. World Health Organization. Obesity: Preventing and managing the global epidemic. Report of a WHO convention. Geneva, Switzerland: World Health Organization;2000.13. NHANES III. National Health and Nutrition Examination Survey. Body measurements(Anthropometry) [Internet]. Rockville: National Health and Nutrition Examination Survey;1988. cite 2010 October 22. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/anthro.pdf.14. Karvetti RL, Knuts LR. Validity of the 24-hour dietary recall. J Am Diet Assoc. 1985; 85(11):1437–1442.15. Roza AM, Shizgal HM. The Harris Benedict equation reevaluated: Resting energy requirements and the body cell mass. Am J Clin Nutr. 1984; 40(1):168–182.
Article16. Moran LJ, Ko H, Misso M, Marsh K, Noakes M, Talbot M, et al. Dietary composition in the treatment of polycystic ovary syndrome: A systematic review to inform evidence-based guidelines. J Acad Nutr Diet. 2013; 113(4):520–545.
Article17. Stener-Victorin E, Jedel E, Janson PO, Sverrisdottir YB. Low-frequency electroacupuncture and physical exercise decrease high muscle sympathetic nerve activity in polycystic ovary syndrome. Am J Physiol Regul Integr Comp Physiol. 2009; 297(2):R387–R395.
Article18. Jedel E, Labrie F, Odén A, Holm G, Nilsson L, Janson PO, et al. Impact of electro-acupuncture and physical exercise on hyperandrogenism and oligo/amenorrhea in women with polycystic ovary syndrome: A randomized controlled trial. Am J Physiol Endocrinol Metab. 2011; 300(1):E37–E45.
Article19. Yildiz BO, Knochenhauer ES, Azziz R. Impact of obesity on the risk for polycystic ovary syndrome. J Clin Endocrinol Metab. 2008; 93(1):162–168.
Article20. Raisbeck E. Understanding polycystic ovary syndrome. Nurse Prescr. 2009; 7(9):390–396.
Article21. Lindenbaum C. Polycystic ovarian syndrome. Where genetics and environment collide. Adv Nurse Pract. 2010; 18(2):20–26.22. Badawy A, Elnashar A. Treatment options for polycystic ovary syndrome. Int J Womens Health. 2011; 8(3):25–35.
Article23. Lass N, Kleber M, Winkel K, Wunsch R, Reinehr TH. Effect of lifestyle intervention on features of polycystic ovarian syndrome, metabolic syndrome, and intima-media thickness in obese adolescent girls. J Clin Endocrinol Metab. 2011; 96(11):3533–3540.
Article24. Hoeger KM, Kochman L, Wixom N, Craig K, Miller RK, Guzick DS. A randomized, 48-week, placebo-controlled trial of intensive lifestyle modification and/or metformin therapy in overweight women with polycystic ovary syndrome: A pilot study. Fertil Steril. 2004; 82(2):421–429.
Article25. Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, et al. Positions statement: Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab. 2006; 91(11):4237–4245.26. Lee S, Bacha F, Gungor N, Arslanian SA. Waist circumference is an independent predictor of insulin resistance in black and white youths. J Pediatr. 2006; 148(2):188–194.
Article27. Ornstein RM, Copperman NM, Jacobson MS. Effect of weight loss on menstrual function in adolescents with polycystic ovary syndrome. J Pediatr Adolesc Gynecol. 2011; 24(3):161–165.
Article28. Ahmed EMS, Salem ME, Sweed MS. Effect of lifestyle modifications on polycystic ovarian syndrome symptoms. J Am Sci. 2012; 8(8):535–544.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Metformin and Rosiglitazone in Overweight or Obese Women with Polycystic Ovarian Syndrome
- Effects of Multidisciplinary Lifestyle Modification Program on Health-promoting Behavior, Psychological Distress, Body Composition and Reproductive Symptoms among Overweight and Obese Middle-aged Women
- Inter-ovarian differences in ultrasound markers of ovarian size in women with polycystic ovary syndrome
- Polycystic Ovary Syndrome
- Association between Metabolic Syndrome and Menstrual Irregularity in Middle-Aged Korean Women