Korean J Androl.
2012 Apr;30(1):80-86. 10.5534/kja.2012.30.1.80.
Preliminary Report about the Efficacy of Prototype Pressure Sensor for the Real-Time Intravesical Pressure Monitoring in the Rabbit
- Affiliations
-
- 1Department of Urology, The Catholic University of Korea College of Medicine, Seoul, Korea. ksw1227@catholic.ac.kr
- 2Department of Mechanical Engineering, Sogang University, Seoul, Korea.
- KMID: 2298813
- DOI: http://doi.org/10.5534/kja.2012.30.1.80
Abstract
- PURPOSE
To maintain physiologic intravesical pressure is important in preventing secondary renal functional impairment in patients with voiding problems like neurogenic bladder or severe bladder outlet obstruction. Therefore, if real-time monitoring of the intravesical pressure were possible, physicians could not only monitor voiding status more precisely but also manage patients with voiding problems appropriately to protect renal function. In this study, we evaluate the validity of the prototype intravesical pressure sensor in a rabbit model.
MATERIALS AND METHODS
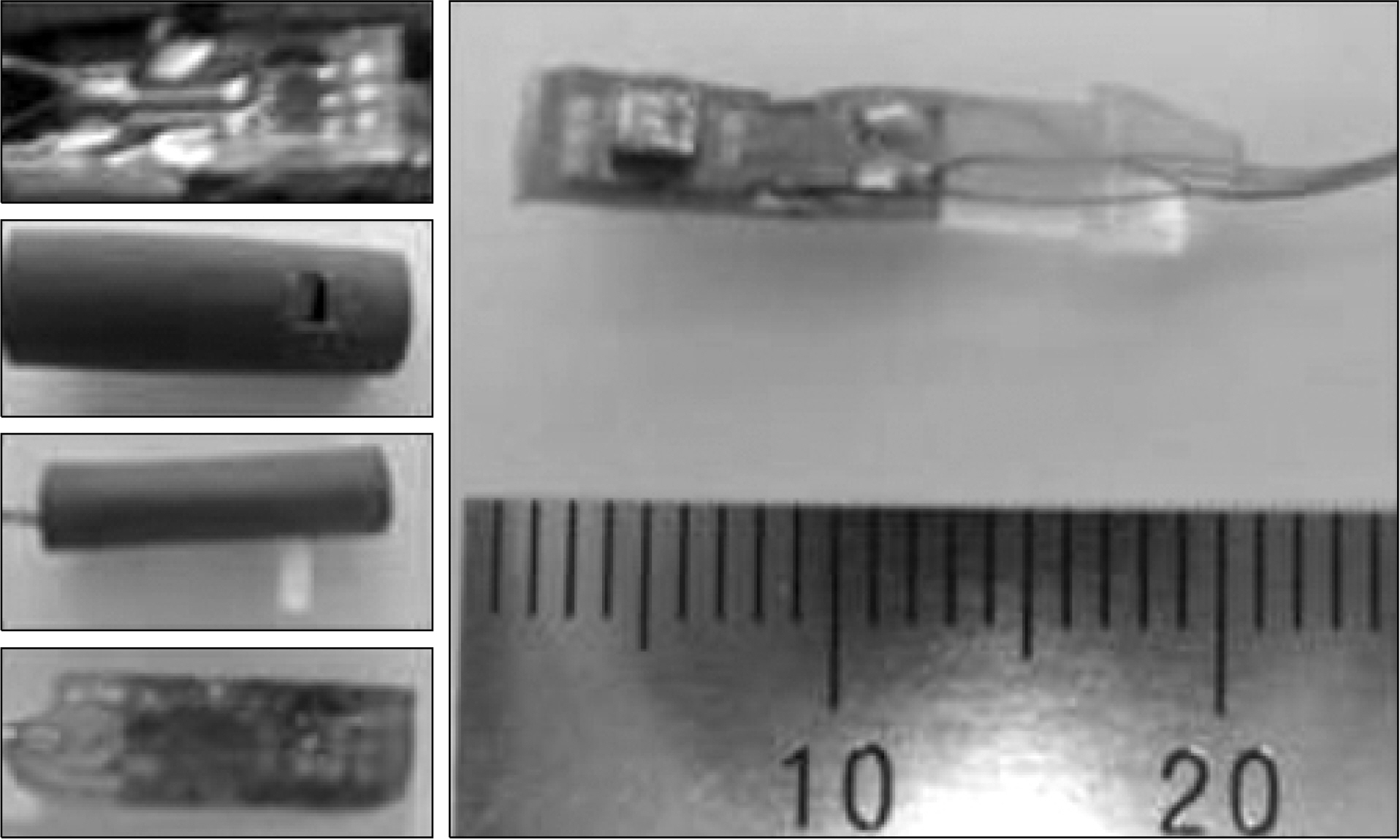
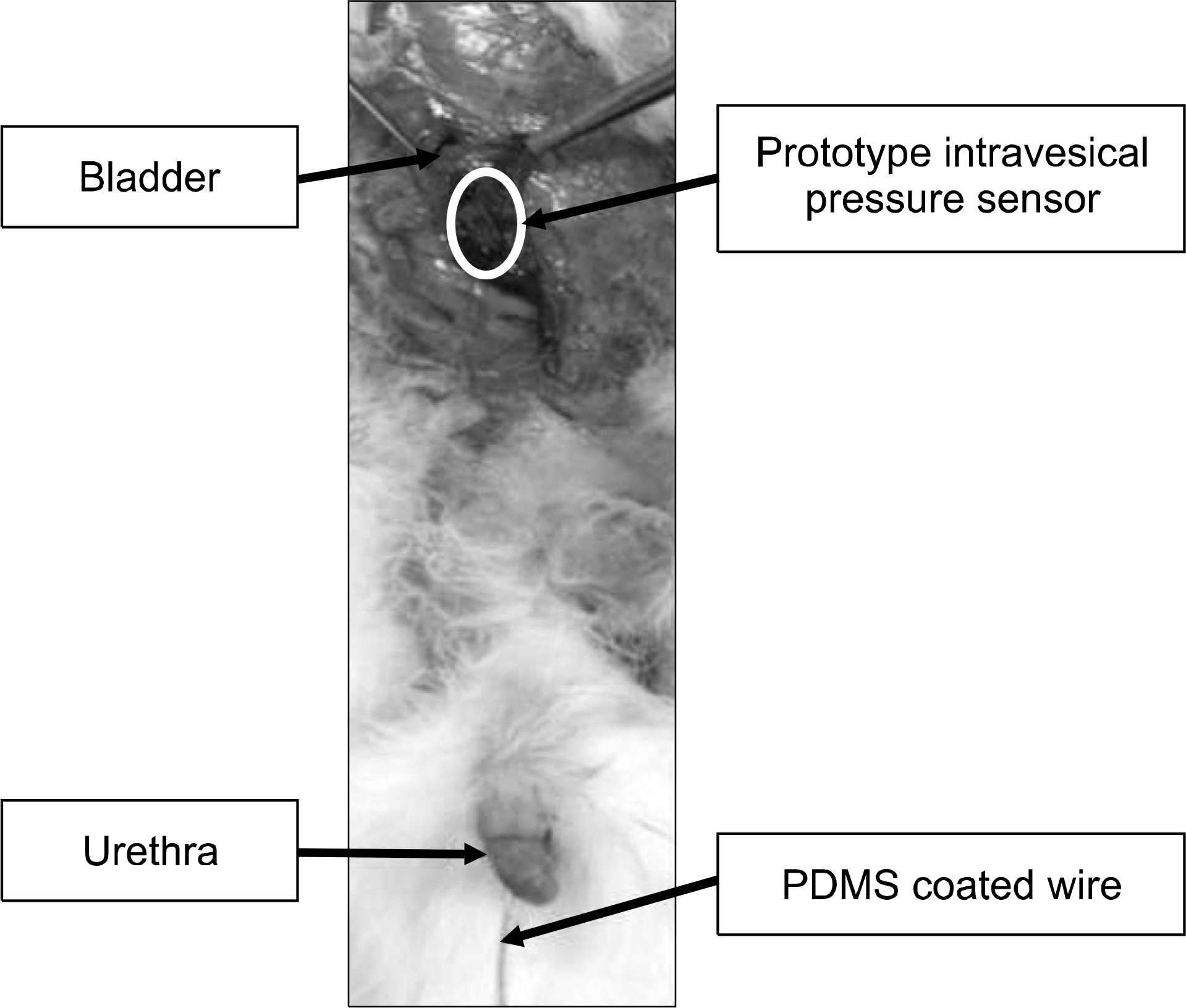
The manufactured prototype intravesical pressure sensor was placed into the intravesical space of each of 3 rabbits. Conventional cystometry was performed and the intravesical pressure was measured by the prototype intravesical pressure sensor at the same time in all of the animals. The measured intravesical pressure by the prototype intravesical pressure sensor was compared with the measured value by conventional cystometry. The reliability between the two methods was determined using cross-table analysis.
RESULTS
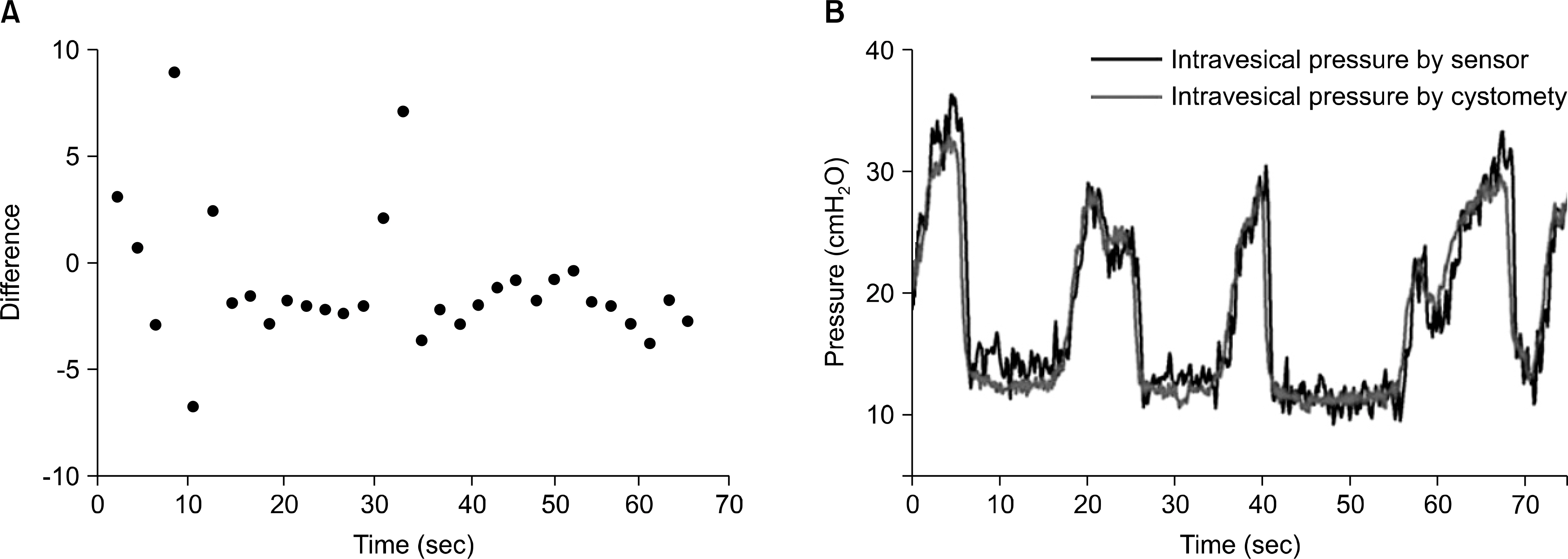
In each of the 3 animals, the index of coincidence was observed as 0.70, 0.79, and 0.77, respectively. This result meant that the intravesical pressure monitoring by the prototype intravesical pressure sensor showed good reproducibility with respect to the continuous intravesical pressure monitoring by conventional cystometry.
CONCLUSIONS
In this study, we demonstrated the reliability of the prototype intravesical pressure sensor to monitor intravesical pressure change compared with the conventional cystometric result. Further investigations to overcome the limitations of the prototype intravesical pressure sensor will be necessary for real clinical application.
Keyword
MeSH Terms
Figure
Reference
-
1). Roehrborn CG. Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Med Clin N Am. 2011; 95:87–100.
Article2). Bosch JL, Cardozo L, Hashim H, Hilton P, Oelke M, Robinson D. Constructing trials to show whether urodynamic studies are necessary in lower urinary tract dysfunction. Neurourol Urodyn. 2011; 30:735–40.
Article3). Klausner AP, Steers WD. The neurogenic bladder: an update with management strategies for primary care physicians. Med Clin North Am. 2011; 95:111–20.
Article4). Rule AD, Lieber MM, Jacobsen SJ. Is benign prostatic hyperplasia a risk factor for chronic renal failure? J Urol. 2005; 173:691–6.
Article5). Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. International Continence Society. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002; 21:261–74.
Article6). Radley SC, Rosario DJ, Chapple CR, Farkas AG. Conventional and ambulatory urodynamic findings in women with symptoms suggestive of bladder overactivity. J Urol. 2001; 166:2253–8.
Article7). Corona-Quintanilla DL, Castelán F, Fajardo V, Manzo J, Martínez-Gómez M. Temporal coordination of pel-vic and perineal striated muscle activity during micturition in female rabbits. J Urol. 2009; 181:1452–8.
Article8). Fletter PC, Majerus S, Cong P, Damaser MS, Ko WH, Young DJ, et al. Wireless micromanometer system for chronic bladder pressure monitoring. The 6th International Conference on Networked Sensing System, Pittsburgh, USA. 2009. 228–31.
Article9). Kadhiresan K, Carlson G. The role of implantable sensors for management of heart failure. Stud Health Technol Inform. 2004; 108:219–27.10). Renard E. Implantable continuous glucose sensors. Curr Diabetes Rev. 2008; 4:169–74.
Article11). Renard E, Costalat G, Chevassus H, Bringer J. Artificial beta-cell: clinical experience toward an implantable closed-loop insulin delivery system. Diabetes Metab. 2006; 32:497–502.12). Hao Y, Foster R. Wireless body sensor networks for health-monitoring applications. Physiol Meas. 2008; 29:R27–56.
Article13). Kakaday T, Hewitt AW, Voelcker NH, Li JS, Craig JE. Advances in telemetric continuous intraocular pressure assessment. Br J Ophthalmol. 2009; 93:992–6.
Article14). Seif C, Herberger B, Cherwon E, Martinez Portillo FJ, Molitor M, Stieglitz T, et al. Urinary bladder volumetry by means of a single retrosymphysically implantable ultrasound unit. Neurourol Urodyn. 2004; 23:680–4.
Article15). Young DJ. Wireless micromanometer system for chronic bladder pressure monitoring. The 5th IEEE International Conference on Nano/Micro engineered and Molecular Systems, Xiamen, China. 2010. 604–7.16). Lee DS, Kim SJ, Sohn DW, Yoo JM, Choi BK, Lee MK, et al. Measurement of bladder volume using an implantable volume sensor in rats. Korean J Androl. 2010; 28:169–74.17). Bates CP, Whiteside CG, Turner-Warwick R. Synchronous cine-pressure-flow-cysto-urethrography with special reference to stress and urge incontinence. Br J Urol. 1970; 42:714–23.
Article18). Gorton E, Stanton S. Women's attitudes to urodynamics: a questionnaire survey. Br J Obstet Gynaecol. 1999; 106:851–6.
Article19). Webb RJ, Ramsden PD, Neal DE. Ambulatory monitoring and electronic measurement of urinary leakage in the diagnosis of detrusor instability and incontinence. Br J Urol. 1991; 68:148–52.
Article20). Heslington K, Hilton P. Ambulatory monitoring and conventional cystometry in asymptomatic female volunteers. Br J Obstet Gynaecol. 1996; 103:434–41.
Article21). Mills IW, Noble JG, Brading AF. Radiotelemetered cystometry in pigs: validation and comparison of natural filling versus diuresis cystometry. J Urol. 2000; 164:1745–50.
Article22). Shaw MB, Herndon CD, Cain MP, Rink RC, Kaefer M. A porcine model of bladder outlet obstruction incorporating radio-telemetered cystometry. BJU Int. 2007; 100:170–4.
Article23). Tan R, McClure T, Lin CK, Jea D, Dabiri F, Massey T, et al. Development of a fully implantable wireless pressure monitoring system. Biomed Microdevices. 2009; 11:259–64.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristic Evaluation of Pressure Mapping System for Patient Position Monitoring in Radiation Therapy
- Application of an Intraoperative Neuromonitoring System Using a Surface Pressure Sensor in Parotid Surgery: A Rabbit Model Study
- Development of a Novel Intraoperative Neuromonitoring System Using a Surface Pressure Sensor to Detect Muscle Movement: A Rabbit Model Study
- Change of Intra-abdominal Pressure on Daily Activities in Patients with Spinal Cord Injury
- Insole Pressure Sensors to Assess Post-Stroke Gait