Korean Circ J.
2010 Feb;40(2):90-93. 10.4070/kcj.2010.40.2.90.
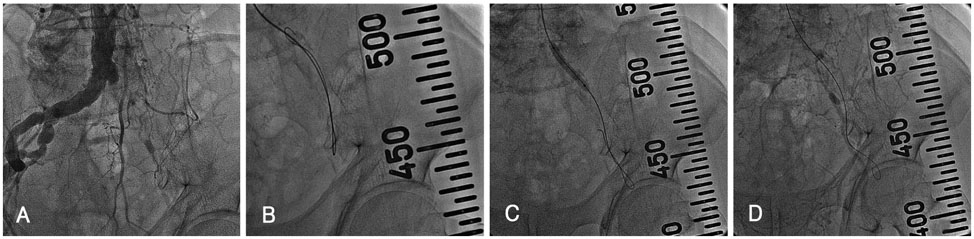
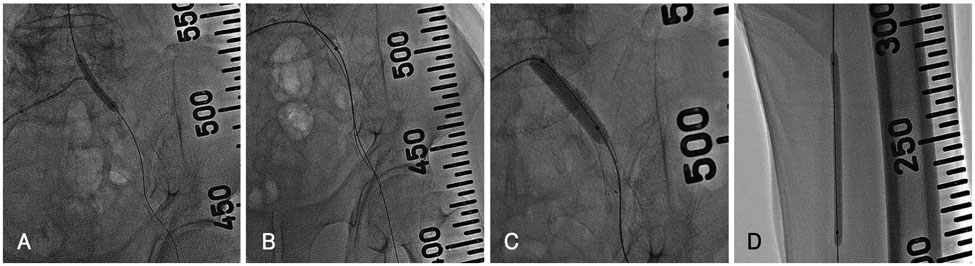
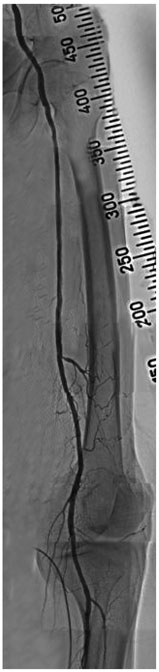
A Dual (Brachial and Contralateral Femoral) Approach for Subintimal Angioplasty of Long Ilio-Femoral Occlusive Disease Including the Iliac Ostium
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Kyung Hee University Medical Center, Seoul, Korea. mylovekw@hanmail.net
- KMID: 2297945
- DOI: http://doi.org/10.4070/kcj.2010.40.2.90
Abstract
- As techniques and device technology have improved, the success rates and long patency of ilio-femoral occlusive disease have also improved. In the case of extensive iliac occlusive disease, however, wire passage and handling remain a challenge due to the relatively weak guiding catheter backup support with the contralateral femoral approach. There has been no report on methods to overcome this problem. We performed a successful percutaneous translunimal angioplasty for long ilio-femoral occlusive disease including the iliac ostium by a dual approach including simultaneous brachial and contralateral femoral arteries for subintimal angioplasty.
Figure
Reference
-
1. Dormandy JA, Rutherford RB. Management of peripheral arterial disease (PAD): TransAtlantic InterSociety Consensus (TASC). J Vasc Surg. 2000. 31:S1–S296.2. Rutherford RB. Options in the surgical management of aortoiliac occlusive disease: a changing perspective. Cardiovasc Surg. 1999. 7:5–12.3. Whiteley MS, Ray-Chaudhuri SB, Galland RB. Changing patterns in aortoiliac reconstruction: a 7-year audit. Br J Surg. 1996. 83:1367–1369.4. Upchurch GR, Dimick JB, Wainess RM, et al. Diffusion of new technology in health care: the case of aorto-iliac occlusive disease. Surgery. 2004. 136:812–818.5. Kashyap VS, Pavkov ML, Bena JF, et al. The management of severe aortoiliac occlusive disease: endovascular therapy rivals open reconstruction. J Vasc Surg. 2008. 48:1451–1457.6. Dyet JF, Gaines PA, Nicholson AA, et al. Treatment of chronic iliac artery occlusions by means of percutaneous endovascular stent placement. J Vasc Interv Radiol. 1997. 8:349–353.7. Henry M, Amor M, Ethevenot G, Henry I, Mentre B, Tzvetanov K. Percutaneous endoluminal treatment of iliac occlusions: long term follow-up in 105 patients. J Endovasc Surg. 1998. 5:228–235.8. Uher P, Nyman U, Lindh M, Lindblad B, Ivancev K. Long-term results for stenting chronic iliac artery occlusions. J Endovasc Ther. 2002. 9:67–75.9. Carnevale FC, De Blas M, Merino S, Egana JM, Caldas JG. Percutaneous endovascular treatment of chronic iliac artery occlusion. Cardiovasc Intervent Radiol. 2004. 27:447–452.10. Lee SH, Park HS, Jang SY, et al. A case of peripheral revascularization via the radial artery using devices designed for percutaneous coronary intervention. Korean Circ J. 2008. 38:671–673.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Recanalization of a Long Superficial Femoral Artery Occlusion by Retrograde Subintimal Angioplasty After a Failed Antegrade Subintimal Approach
- Subintimal Stent Placement in Patients with Long Segment Occlusion of the Iliac Artery
- Endovascular Management for Chronic Steno-occlusion of Iliac and Femoral Arteries
- Effects of Subintimal Angioplasty in Patients with Ischemic Arterial Disease of Lower Extremities
- The Relation between Distal Runoff and Clinical Outcome after Aorto-iliac Reconstruction Surgery